Ara Darzi Antibiotic Resistance Deadlier Than Cancer?
Ara Darzi on why antibiotic resistance could be deadlier than cancer – it’s a chilling thought, isn’t it? We often hear about the cancer crisis, but what if a silent killer, one we’re inadvertently fostering through overuse of antibiotics, surpasses it in lethality? This isn’t just hypothetical; leading experts like Lord Darzi are sounding the alarm, highlighting the urgent need to understand and combat the growing threat of antibiotic-resistant infections.
This post delves into his perspective, comparing the mortality rates of antibiotic resistance and cancer, exploring the underlying mechanisms, and examining the socioeconomic and public health implications.
The implications are staggering. We’ll examine the stark statistics – comparing mortality rates, projecting future trends, and analyzing the economic burden of both antibiotic resistance and cancer. We’ll then delve into the biological mechanisms, exploring the similarities and differences in how resistance develops in bacteria and how cancer progresses. Finally, we’ll discuss preventative measures, treatment strategies, and the crucial role of research and development in turning the tide against this looming crisis.
Ara Darzi’s Expertise and Perspective on Antibiotic Resistance
Lord Ara Darzi of Denham is a highly influential figure in global healthcare, renowned for his expertise in surgery, healthcare policy, and global health. His unique perspective, combining surgical experience with a deep understanding of healthcare systems and policy, makes him uniquely positioned to address the looming threat of antibiotic resistance. His work consistently emphasizes the interconnectedness of various healthcare challenges and the need for innovative, system-wide solutions.Ara Darzi’s career is marked by significant contributions to surgical innovation and healthcare reform.
Lord Ara Darzi’s warnings about antibiotic resistance eclipsing cancer in lethality are chilling. It’s a sobering thought, especially when considering the fragility of our systems – for example, the news that six Minnesota counties have 515 duplicate registrations on voter rolls, as a watchdog alleges , highlights how easily things can go wrong. Such vulnerabilities underscore the need for robust systems to combat both public health crises like antibiotic resistance and administrative issues impacting our democracy.
We need to address both, urgently.
He is a renowned surgeon, having held prominent positions at Imperial College London, where he served as Director of the Institute of Global Health Innovation. His work extends beyond the operating room; he’s been deeply involved in shaping healthcare policy at national and international levels, advising governments and organizations on improving healthcare delivery and outcomes. His influence is evident in numerous publications and policy recommendations, many directly or indirectly addressing the challenges posed by infectious diseases.
Ara Darzi’s Relevant Work and Publications
While a comprehensive list of Lord Darzi’s publications would be extensive, several examples illustrate his focus on areas relevant to antibiotic resistance. His work often emphasizes the need for improved infection control measures within healthcare settings, a critical component in combating the spread of antibiotic-resistant bacteria. He has actively promoted the development and implementation of innovative technologies and strategies to enhance healthcare delivery and improve patient safety, areas directly relevant to preventing and managing infections.
For instance, his involvement in projects focusing on improving surgical techniques and post-operative care directly impacts infection rates and, consequently, the demand for antibiotics. His research and advocacy frequently highlight the need for a multi-faceted approach to tackling healthcare challenges, including antibiotic resistance. His publications often emphasize the societal and economic impact of failing to address these challenges effectively.
Ara Darzi’s Perspective on Antibiotic Resistance vs. Cancer
Given his extensive experience, Lord Darzi likely views antibiotic resistance as a threat of comparable, if not greater, magnitude than cancer. While cancer remains a significant global health challenge, antibiotic resistance poses a unique threat because it undermines our ability to treat a wide range of bacterial infections. The consequences of widespread antibiotic resistance could be catastrophic, potentially reversing decades of progress in healthcare and leading to a resurgence of previously manageable infections.
This is unlike cancer, where advances in treatment continue, albeit at a slower pace than the development of antibiotic resistance. Lord Darzi’s emphasis on preventative measures and systems-level thinking likely aligns with the need for a comprehensive, global strategy to combat antibiotic resistance, which is far more challenging to tackle than cancer, due to its multifaceted nature involving public health, individual behaviors, and pharmaceutical development.
He would likely stress the urgent need for collaborative efforts involving governments, healthcare professionals, pharmaceutical companies, and individuals to mitigate this impending crisis.
Lord Darzi’s warnings about antibiotic resistance surpassing cancer in lethality really hit home. It’s a chilling thought, especially considering the legal battles surrounding healthcare – you can find resources on navigating the US legal system via helpful guides like these us court website links , which might be relevant if you’re facing issues related to medical negligence or pharmaceutical litigation.
The implications of unchecked antibiotic resistance are far-reaching, demanding urgent attention and effective solutions.
Comparing Mortality Rates

The looming threat of antibiotic resistance often overshadows other global health crises. While cancer remains a significant cause of death worldwide, the rapid escalation of antibiotic-resistant infections presents a unique and potentially more devastating challenge. A direct comparison of mortality rates helps illuminate the severity of this emerging public health emergency. Accurate data is crucial for effective resource allocation and policy development to combat both threats effectively.
Directly comparing mortality rates between antibiotic resistance and cancer requires careful consideration of data limitations. Precise figures for antibiotic-resistant infections are challenging to obtain due to inconsistent reporting and diagnostic capabilities across different regions. Cancer mortality data, while more readily available, varies based on cancer type, access to treatment, and socioeconomic factors. Nevertheless, available data offers a concerning glimpse into the comparative impact of these two major health challenges.
Global Mortality Rates: Antibiotic Resistance vs. Cancer
The following table provides an estimated comparison of mortality rates, acknowledging the inherent uncertainties in data collection for antibiotic resistance. These figures represent a snapshot in time and are subject to change. Note that ‘Antibiotic-Resistant Infections’ encompasses a broad range of infections caused by resistant bacteria, making precise comparisons challenging.
| Disease | Mortality Rate (per 100,000) | Age Group Most Affected | Geographic Distribution |
|---|---|---|---|
| Cancer (All Types) | 150-200 (varies significantly by region and cancer type) | 65+ (varies significantly by cancer type) | Globally prevalent, with variations in incidence and mortality rates across regions due to access to healthcare and socioeconomic factors. |
| Antibiotic-Resistant Infections | 700,000 (estimated deaths in 2019, projected to increase significantly) | Varied, with significant impact on vulnerable populations (young children, elderly, immunocompromised) | Globally prevalent, with higher rates observed in low- and middle-income countries due to factors such as limited access to healthcare, sanitation, and hygiene. |
Projected Mortality Rates: The Next Decade
Projecting mortality rates for both antibiotic resistance and cancer requires considering various factors, including advancements in medical treatment, public health interventions, and demographic shifts. The projections below represent reasonable estimations based on current trends, but significant variations are possible.
Experts predict a substantial increase in deaths attributable to antibiotic resistance within the next decade. The World Health Organization (WHO) estimates that without significant intervention, antibiotic-resistant infections could cause 10 million deaths annually by 2050. Cancer mortality rates are also projected to rise, driven by aging populations and increasing incidence rates of certain cancers. However, improvements in cancer screening, diagnosis, and treatment are expected to mitigate the rate of increase to some degree.
The exact figures remain uncertain and are subject to continuous research and epidemiological monitoring.
Projected Growth in Mortality Rates: The Next 20 Years
The following description depicts a hypothetical graph illustrating the projected growth in mortality rates for antibiotic-resistant infections and cancer over the next 20 years. The graph would use a line graph format, with time (years) on the x-axis and mortality rate (per 100,000) on the y-axis. Two lines would represent the projected mortality rates for each disease. The line representing antibiotic-resistant infections would show a steeper upward trajectory than the line for cancer, reflecting the faster projected growth in mortality.
The graph would highlight the significant difference in the rate of increase between the two diseases, emphasizing the potentially greater threat posed by antibiotic resistance.
For example, the graph might show a starting point of 700,000 deaths annually from antibiotic resistance in 2024, increasing to potentially over 2 million by 2044. Cancer deaths might increase from a baseline of, for instance, 10 million to 12 million over the same period. This visual representation would underscore the urgency of addressing antibiotic resistance as a major global health threat, surpassing the projected growth in cancer mortality within the timeframe considered.
The Mechanisms of Antibiotic Resistance and Cancer Development
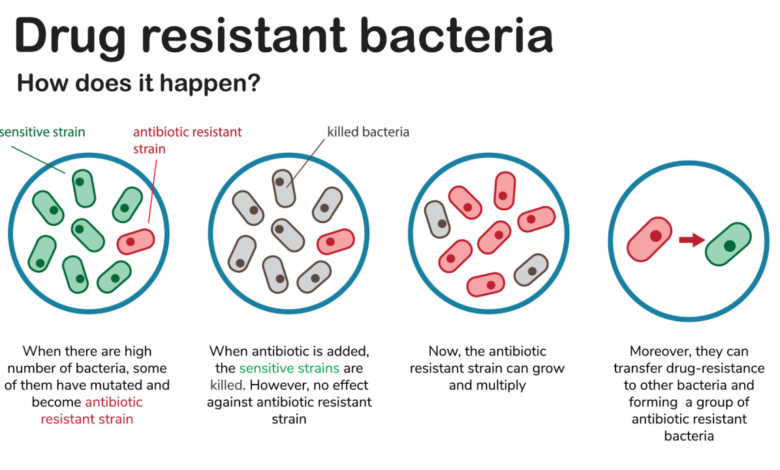
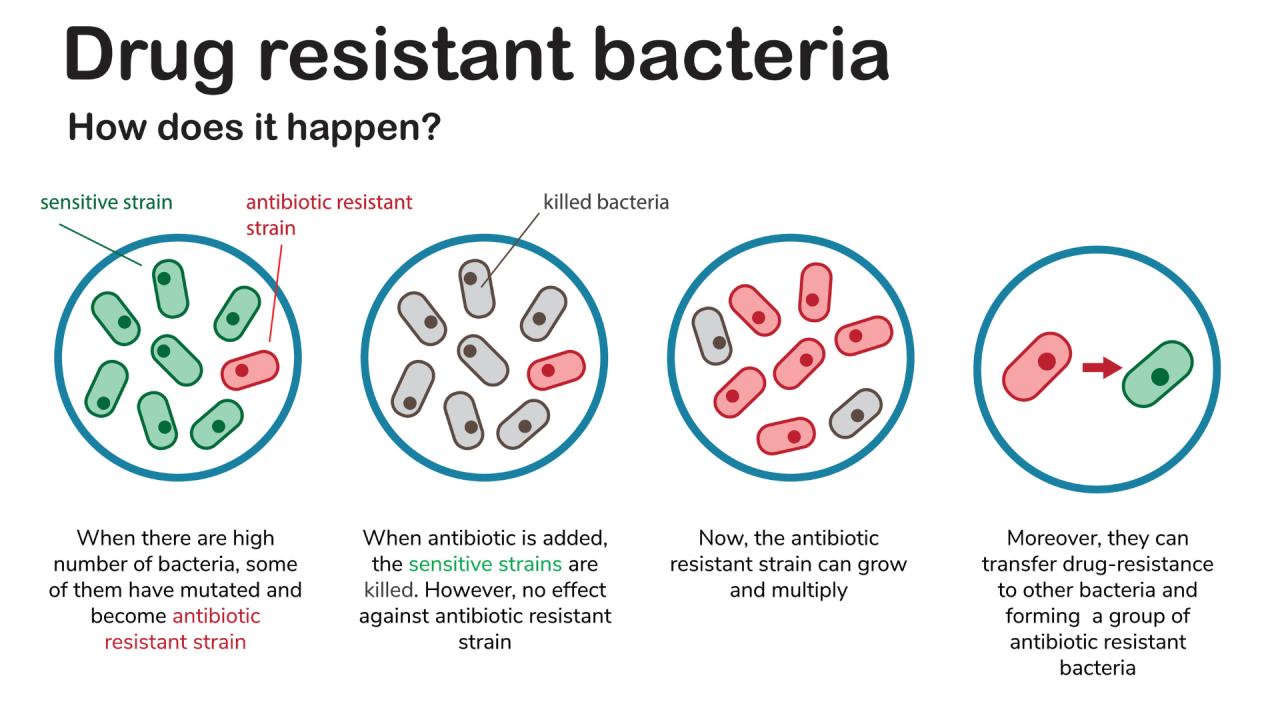
Antibiotic resistance and cancer, while seemingly disparate, share intriguing parallels at the cellular level. Both involve disruptions in fundamental biological processes, leading to uncontrolled proliferation and survival of affected cells. Understanding the mechanisms driving each process reveals surprising commonalities, highlighting the interconnectedness of these major global health threats.The development of antibiotic resistance is a complex process driven by the evolution of bacteria in response to antibiotic pressure.
Bacteria employ various strategies to evade the effects of antibiotics. These mechanisms are often encoded in their DNA and can be transferred between bacteria, facilitating the rapid spread of resistance.
Mechanisms of Antibiotic Resistance
Bacteria develop resistance through several key mechanisms. One common strategy is the inactivation of antibiotics. Bacteria produce enzymes that chemically modify or degrade antibiotics, rendering them ineffective. For example, β-lactamases are enzymes that break down β-lactam antibiotics like penicillin. Another mechanism is alteration of the antibiotic target site.
Bacteria can mutate the genes encoding proteins that are the targets of antibiotics, preventing the antibiotic from binding and exerting its effect. Changes in the bacterial ribosome, for example, can confer resistance to aminoglycoside antibiotics. Furthermore, bacteria can reduce antibiotic accumulation by altering their cell membranes to decrease antibiotic permeability or by increasing efflux pumps, which actively expel antibiotics from the cell.
Finally, some bacteria develop alternative metabolic pathways to bypass the antibiotic’s effect on their essential metabolic processes. The combination of these mechanisms, often acting synergistically, can lead to multi-drug resistance, making infections extremely difficult to treat.
Comparison of Antibiotic Resistance and Cancer Development
Both antibiotic resistance and cancer involve dysregulation of cellular processes that govern growth and survival. In antibiotic resistance, this dysregulation is manifested in the bacterial cell’s ability to overcome the lethal effects of antibiotics. In cancer, the dysregulation manifests as uncontrolled cell growth and division, leading to tumor formation. While the specific molecular mechanisms differ, both processes involve mutations in genes controlling cell division, DNA repair, and apoptosis (programmed cell death).
In antibiotic resistance, mutations lead to altered antibiotic targets or increased efflux pump activity. In cancer, mutations can activate oncogenes (genes promoting cell growth) or inactivate tumor suppressor genes (genes inhibiting cell growth). The resulting uncontrolled proliferation is a common thread between the two.
Common Risk Factors for Antibiotic Resistance and Cancer
Several factors contribute to both antibiotic resistance and increased cancer susceptibility. These overlapping risk factors underscore the interconnectedness of these health challenges. For instance, immunocompromised individuals are more susceptible to both infections (leading to increased antibiotic use and resistance selection) and cancer. Similarly, exposure to certain environmental toxins and carcinogens can increase the risk of both cancer and bacterial infections, potentially driving the selection of antibiotic-resistant strains.
Lord Darzi’s warning about antibiotic resistance surpassing cancer in lethality really hit home. It made me think about the wider societal pressures; how can we expect people to prioritize health when they’re struggling financially, as highlighted in this insightful article on Britain’s big squeeze middle class and minimum wage ? Access to healthcare and preventative measures are crucial in fighting antibiotic resistance, and financial strain undermines that entirely.
Genetic predisposition also plays a role; individuals with inherited genetic mutations that affect DNA repair or immune function are at higher risk of both cancer and developing infections that require antibiotic treatment, contributing to the spread of resistance. Furthermore, prolonged or inappropriate use of antibiotics creates selective pressure for resistant bacteria, while factors such as age, lifestyle choices (e.g., diet, smoking), and exposure to radiation can influence both cancer risk and the likelihood of developing infections requiring antibiotic treatment.
The Socioeconomic Impact of Antibiotic Resistance and Cancer
The escalating threat of antibiotic resistance casts a long shadow beyond individual health, significantly impacting global socioeconomic stability. Its effects ripple through healthcare systems, labor markets, and national economies, creating a burden comparable to, and in some ways exceeding, the socioeconomic impact of cancer. Understanding this multifaceted impact is crucial for developing effective strategies to combat this growing crisis.The economic burden of antibiotic-resistant infections is substantial and multifaceted.
It encompasses direct healthcare costs, indirect costs stemming from lost productivity, and the devastating economic consequences of premature mortality.
Healthcare Costs Associated with Antibiotic Resistance
The treatment of antibiotic-resistant infections is significantly more expensive than treating infections caused by susceptible bacteria. Longer hospital stays, the need for more potent (and often more costly) antibiotics, and increased use of intensive care resources all contribute to inflated healthcare expenditures. For example, a study in the United States estimated that the annual healthcare costs associated with antibiotic-resistant infections exceed $20 billion.
This figure reflects not only the direct costs of treatment but also the indirect costs associated with managing outbreaks and implementing infection control measures. Furthermore, the development of new antibiotics is a costly and time-consuming process, further exacerbating the financial strain on healthcare systems worldwide.
Lost Productivity Due to Antibiotic-Resistant Infections
Antibiotic-resistant infections often lead to prolonged illness, disability, and even death, resulting in significant losses in productivity. Individuals affected by these infections may be unable to work, leading to lost wages and reduced economic output. This impact extends beyond the individual, affecting families, communities, and national economies. The World Health Organization estimates that the global economic impact of lost productivity due to antimicrobial resistance could reach trillions of dollars annually.
This loss of productivity is particularly impactful in developing countries, where a significant portion of the population relies on informal employment and lacks access to robust social safety nets.
Mortality-Related Economic Losses from Antibiotic Resistance
The premature deaths caused by antibiotic-resistant infections represent a profound economic loss. These losses encompass not only the loss of potential future earnings but also the associated costs of funeral expenses, bereavement support, and the broader social and economic consequences of losing productive members of society. The value of a statistical life, a measure used by economists to quantify the economic cost of premature death, is often substantial, highlighting the significant economic burden associated with antibiotic-resistant infections.
The premature death of young adults, in particular, represents a significant loss of human capital and future economic contributions.
Comparison of Socioeconomic Impacts: Antibiotic Resistance vs. Cancer
While both antibiotic resistance and cancer pose significant socioeconomic burdens, the nature and scale of these burdens differ. Cancer treatment and care are expensive, but effective treatments exist for many types of cancer, leading to improved survival rates and reduced long-term economic consequences. However, the lack of effective treatments for many antibiotic-resistant infections, coupled with the rapid spread of resistance, presents a more daunting challenge.
The potential for catastrophic consequences from unchecked antibiotic resistance—including the collapse of modern medicine’s ability to perform routine surgeries and treat common infections—exceeds the currently manageable socioeconomic burden of cancer.
Long-Term Economic Consequences of Unchecked Antibiotic Resistance, Ara darzi on why antibiotic resistance could be deadlier than cancer
The long-term economic consequences of unchecked antibiotic resistance are potentially catastrophic. Without effective interventions, the rising prevalence of antibiotic-resistant infections could overwhelm healthcare systems, cripple economies, and threaten global health security. The potential for a return to a pre-antibiotic era, where common infections could become life-threatening, is a stark reality. This scenario would have devastating consequences for healthcare systems, economies, and societies worldwide.
The development and implementation of effective strategies to combat antibiotic resistance are therefore not just public health imperatives, but also critical economic necessities.
Preventive Measures and Treatment Strategies
Combating antibiotic resistance requires a multifaceted approach encompassing both preventative measures to curb the spread of resistant infections and innovative treatment strategies to manage existing cases. The effectiveness of these strategies hinges on a global commitment to responsible antibiotic use and the development of new therapeutic approaches.Preventing the spread of antibiotic-resistant infections is crucial to mitigating the growing threat.
This involves a combination of individual responsibility and robust public health initiatives.
Preventive Measures to Reduce Antibiotic-Resistant Infections
Effective prevention relies on minimizing the unnecessary use of antibiotics, improving hygiene practices, and implementing infection control measures in healthcare settings. The overuse of antibiotics fuels the selection and spread of resistant bacteria. Therefore, responsible antibiotic stewardship programs are paramount. These programs promote the appropriate prescription and use of antibiotics, reserving them for bacterial infections and avoiding their use for viral illnesses like the common cold or flu.
- Hand Hygiene: Frequent and thorough handwashing with soap and water or an alcohol-based hand sanitizer is the single most effective measure to prevent the spread of infections, including those caused by antibiotic-resistant bacteria. This simple act significantly reduces the transmission of bacteria from person to person.
- Infection Control in Healthcare Settings: Hospitals and other healthcare facilities must maintain stringent infection control protocols. This includes proper sterilization of equipment, isolation of infected patients, and adherence to guidelines for personal protective equipment (PPE) use by healthcare workers. These protocols are designed to prevent the spread of antibiotic-resistant bacteria within these environments.
- Vaccination: Vaccination programs against bacterial infections reduce the overall need for antibiotics, thereby limiting the selection pressure that drives antibiotic resistance. For instance, widespread vaccination against pneumococcal pneumonia significantly decreases the incidence of this serious bacterial infection.
- Improved Sanitation and Hygiene: Access to clean water and sanitation facilities plays a critical role in preventing the spread of infections. Improved sanitation reduces exposure to antibiotic-resistant bacteria in the environment, decreasing the likelihood of infection.
- Responsible Antibiotic Use in Agriculture: The widespread use of antibiotics in livestock farming contributes significantly to the development and spread of antibiotic resistance. Reducing the use of antibiotics in agriculture is essential to mitigate this problem. This could involve exploring alternative methods to control bacterial infections in animals.
Treatment Strategies for Antibiotic-Resistant Infections Compared to Cancer Treatment
Treatment of antibiotic-resistant infections presents significant challenges. Unlike cancer, where a wide range of targeted therapies exist, options for antibiotic-resistant infections are limited. Current strategies focus on alternative antibiotics, combination therapies, and novel approaches.
- Alternative Antibiotics: The search for new antibiotics with different mechanisms of action is crucial. However, the development of new antibiotics is a slow and expensive process.
- Combination Therapies: Using multiple antibiotics simultaneously can sometimes overcome resistance mechanisms. This approach aims to exploit the synergistic effects of different drugs to eliminate resistant bacteria.
- Bacteriophages: Bacteriophages are viruses that specifically infect and kill bacteria. They offer a potential alternative treatment for antibiotic-resistant infections. Research is ongoing to explore their therapeutic potential.
- Immunotherapies: Boosting the body’s own immune system to fight bacterial infections is another promising avenue. This approach aims to enhance the immune response to clear resistant bacteria more effectively.
Cancer treatment, in contrast, utilizes a broader range of approaches, including surgery, chemotherapy, radiation therapy, targeted therapies, and immunotherapy. The diversity of cancer treatment options reflects the complexity of the disease and the continuous development of new therapeutic strategies. However, the similarities lie in the need for personalized approaches based on the specific characteristics of the infection or cancer.
Public Health Campaign Strategy to Raise Awareness about Antibiotic Resistance
A comprehensive public health campaign is needed to raise awareness about antibiotic resistance and promote responsible antibiotic use. This campaign should target healthcare professionals, the general public, and policymakers.
- Key Messaging Points:
- Antibiotics are powerful medicines, but their effectiveness is threatened by resistance.
- Antibiotics only work against bacterial infections, not viral infections like colds and flu.
- Always follow your doctor’s instructions when taking antibiotics.
- Never share or save antibiotics for later use.
- Practicing good hygiene can help prevent the spread of infections.
- Dissemination Methods:
- Public service announcements (PSAs) on television, radio, and social media.
- Educational materials for healthcare professionals and the public.
- Partnerships with community organizations and schools.
- Interactive websites and mobile apps.
- Social media campaigns using hashtags and engaging content.
Research and Development in Combating Antibiotic Resistance: Ara Darzi On Why Antibiotic Resistance Could Be Deadlier Than Cancer
The escalating threat of antibiotic resistance demands a concerted global effort in research and development to discover and deploy novel antimicrobial agents and alternative therapies. The current pipeline of new antibiotics is alarmingly thin, highlighting the urgent need for innovative approaches and increased investment in this critical area. Success hinges on a multi-pronged strategy involving both the development of new drugs and the exploration of alternative methods to combat resistant infections.The development of new antimicrobial agents faces significant challenges.
The lengthy and expensive process of drug discovery and development, coupled with the inherent difficulty of identifying novel targets in bacteria and the emergence of resistance mechanisms, presents a formidable hurdle. Furthermore, the limited financial incentives for pharmaceutical companies to invest in antibiotic development, given the relatively short course of treatment and the potential for rapid resistance development, further exacerbates the problem.
However, opportunities exist in leveraging advanced technologies and innovative approaches to overcome these obstacles.
Novel Antibiotic Discovery Strategies
Researchers are exploring various avenues to discover new antibiotics. This includes high-throughput screening of vast chemical libraries, utilizing artificial intelligence and machine learning to predict and design novel antimicrobial compounds, and investigating natural sources such as soil microbes and marine organisms for new antibiotic leads. For example, researchers are using advanced genomics techniques to identify novel bacterial targets that are less susceptible to resistance mechanisms.
The development of new antibiotics based on different mechanisms of action, targeting bacterial processes other than cell wall synthesis or protein synthesis, is also a promising area of research. This approach reduces the likelihood of cross-resistance with existing antibiotics.
Alternative Therapies to Antibiotics
Given the challenges in developing new antibiotics, significant research is underway exploring alternative therapies. These include phage therapy, which utilizes bacteriophages (viruses that infect bacteria) to kill specific bacterial strains; immunotherapy, which harnesses the power of the immune system to combat bacterial infections; and the development of new vaccines to prevent bacterial infections in the first place. Phage therapy, for instance, has shown promise in treating infections caused by multi-drug resistant bacteria in clinical trials, although further research is needed to establish its widespread applicability.
Immunotherapeutic approaches aim to boost the host’s immune response to effectively clear bacterial infections, offering a potential alternative to direct antimicrobial action.
Accelerating Antibiotic Development Through Innovative Approaches
Several innovative approaches are being explored to accelerate the development of new antibiotics and reduce the associated costs. These include repurposing existing drugs for antimicrobial use, developing combination therapies to prevent or delay the emergence of resistance, and exploring novel drug delivery systems to improve efficacy and reduce toxicity. Repurposing existing drugs can significantly reduce the time and cost required for development, while combination therapies leverage the synergistic effects of multiple drugs to overcome resistance.
Innovative drug delivery systems, such as nanoparticles, can improve the targeted delivery of antibiotics, minimizing side effects and maximizing efficacy. For example, researchers are investigating the use of nanoparticles to deliver antibiotics directly to infected tissues, enhancing their effectiveness and reducing the overall dose required.
The prospect of antibiotic resistance surpassing cancer in terms of mortality is a stark wake-up call. Lord Darzi’s perspective, backed by compelling data, underscores the urgency of the situation. While the fight against cancer remains paramount, we must equally prioritize the development of new antibiotics, responsible antibiotic use, and public health campaigns to educate the population. Ignoring this threat will have devastating consequences, not only in terms of lives lost but also in the crippling socioeconomic burden it will impose.
The time to act is now, before antibiotic resistance becomes an unstoppable force.





