Britains £200bn QE Loss How Should We Proceed?
How should britain handle 200bn in quantitative easing losses – Britain’s £200bn QE Loss: How Should We Proceed? This colossal figure, the result of years of quantitative easing, isn’t just a number on a spreadsheet; it’s a potential economic earthquake. We’re facing a serious challenge, one that demands careful consideration of its implications for the national debt, inflation, and the future of public services. This isn’t just about dry economic figures; it’s about the real-world impact on all of us.
Let’s dive into the complexities of this situation and explore potential solutions.
The sheer scale of the loss is staggering. It’s the result of the Bank of England’s efforts to stimulate the economy following the 2008 financial crisis and the COVID-19 pandemic. Buying government and corporate bonds artificially lowered interest rates, but now those bonds are worth less than they were when purchased. The question is: how do we, as a nation, navigate this financial storm?
What are the trade-offs between different policy options? And how can we ensure that the burden is shared fairly?
The Scale of the Problem
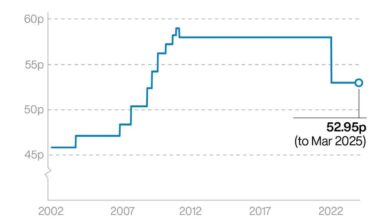
The £200 billion in losses stemming from the Bank of England’s quantitative easing (QE) programme represents a significant challenge for the UK economy. Understanding the scale of these losses requires examining the mechanics of QE and its impact on the national debt. This isn’t simply a matter of accounting; it has real-world implications for future government spending and economic stability.QE, implemented to stimulate the economy after the 2008 financial crisis and again during the pandemic, involved the Bank of England purchasing government and corporate bonds from commercial banks.
This injection of cash into the banking system was intended to lower interest rates and encourage lending. However, the subsequent rise in interest rates has significantly reduced the value of these bonds held by the Bank of England, resulting in substantial unrealised losses.
Composition of QE Losses
The £200 billion figure encompasses losses across various asset classes. A large portion consists of losses on government bonds, reflecting the inverse relationship between bond prices and interest rates. As interest rates have risen, the value of these bonds, purchased at lower rates, has fallen. The losses also include those incurred on corporate bonds, though the exact proportions are not publicly available with complete transparency, making precise breakdown difficult.
The Bank of England’s portfolio also includes other assets, but the bulk of the losses are concentrated in these two main categories.
Impact on National Debt and Borrowing Costs
These losses directly impact the national debt. While they are currently unrealised – meaning the Bank of England hasn’t actually sold the bonds – they represent a potential liability. If the Bank were to sell these bonds at current market prices, it would incur a significant loss, which would then need to be covered by the government, adding to the national debt.
A potential graph illustrating this relationship would show two lines: one representing the growth of the national debt over time and another showing the cumulative QE losses. Initially, the debt line would rise steadily. As QE losses increase, the debt line would experience a steeper upward trajectory. The gap between the two lines would visually represent the potential increase in the national debt should the Bank of England need to sell these assets to offset the losses.
This increased debt could lead to higher future borrowing costs for the government, as lenders demand higher interest rates to compensate for increased risk. For example, if the government needs to borrow more to cover these losses, the increased demand for loans could push interest rates up, making it more expensive for the government to finance its spending in the future.
This scenario is analogous to what happened in the Eurozone sovereign debt crisis of 2010-2012, where concerns about government debt levels led to significantly higher borrowing costs for countries like Greece and Italy.
Economic Impact Assessment
The £200 billion in quantitative easing (QE) losses represent a significant challenge for the UK economy. Understanding the potential short-term and long-term impacts of these losses is crucial for policymakers to develop effective strategies for mitigation and management. This assessment explores the potential inflationary pressures, the implications for government spending, and compares different approaches to handling this financial burden.
Short-Term Inflationary Pressures
The immediate concern stemming from the QE losses is the potential for increased inflationary pressures. The Bank of England’s QE program involved purchasing government bonds, injecting liquidity into the financial system. Reversing this process, or essentially writing off these losses, could lead to a reduction in the money supply. While this might seem counterintuitive to inflation, the impact is complex.
The government might need to raise taxes or cut spending to offset these losses, potentially reducing disposable income and dampening demand. However, the uncertainty surrounding the handling of these losses could also lead to market volatility and increased investor anxiety, potentially driving up prices of goods and services. This could exacerbate existing inflationary pressures, particularly if the government chooses a method that causes sudden market shifts.
So, Britain’s facing a whopping £200bn loss from quantitative easing – how on earth do we tackle that? It’s a seriously complex issue, and honestly, I’ve been trying to wrap my head around it while reading the latest blighty newsletter the return of the good chaps , which actually offered some surprisingly insightful commentary on the economic climate.
Perhaps some of their suggestions on fiscal responsibility could offer a path forward on this QE loss problem. It’s definitely a challenge requiring careful consideration.
For example, a rapid sale of government bonds to recoup some of the losses could flood the market, potentially depressing bond prices and impacting interest rates.
Long-Term Consequences for Government Spending and Public Services
The long-term consequences of the QE losses will significantly impact government spending and the provision of public services. The government faces a difficult choice: absorb the losses directly, potentially leading to reduced spending in other areas; or implement austerity measures to offset the losses, potentially leading to cuts in vital public services like healthcare and education. The scale of the losses necessitates significant fiscal adjustments.
For instance, a decision to absorb the losses could require significant tax increases or reductions in government investment in infrastructure projects. Alternatively, austerity measures could lead to reduced funding for essential public services, potentially impacting their quality and accessibility. The long-term economic impact will depend heavily on the chosen approach and its effect on consumer and business confidence.
Comparison of Approaches to Handling QE Losses, How should britain handle 200bn in quantitative easing losses
The following table compares different approaches to handling the £200 billion in QE losses, considering their short-term and long-term economic impacts, as well as potential risks:
| Approach | Short-term Impact | Long-term Impact | Potential Risks |
|---|---|---|---|
| Absorbing the losses directly | Potential for increased government borrowing and higher interest rates; limited immediate market impact. | Increased national debt; potential for reduced government spending on public services; long-term inflationary pressures depending on how the government finances the losses. | Increased national debt could negatively affect credit rating; potential for political backlash due to reduced public services. |
| Gradual sale of assets | Potential for modest inflationary pressures; slow reduction in the government’s balance sheet. | Reduced national debt; potential for increased government revenue; gradual adjustment to reduced government spending. | Market volatility if the sale is too rapid; potential for losses if asset prices fall; slow pace of debt reduction. |
| Tax increases | Immediate reduction in disposable income; potential for reduced consumer spending and economic slowdown. | Reduced national debt; potential for improved government finances; but potential for long-term economic stagnation if taxes are too high. | Potential for social unrest; reduced economic activity; potential for tax avoidance. |
| Austerity measures | Immediate reduction in government spending; potential for reduced economic growth. | Reduced national debt; potential for improved government finances; but potential for long-term damage to public services and infrastructure. | Potential for social unrest; reduced quality of public services; potential for long-term economic damage. |
Policy Options for Addressing the Losses: How Should Britain Handle 200bn In Quantitative Easing Losses
The £200 billion loss from quantitative easing presents the UK government with a significant fiscal challenge. Several policy options exist to absorb or mitigate these losses, each with its own economic and political ramifications. The choice will depend on a complex balancing act between fiscal responsibility, economic stability, and public acceptance.
Tax Increases
Raising taxes is a direct method of increasing government revenue to offset the QE losses. This could involve increasing income tax, corporation tax, or introducing new taxes on specific sectors or goods. For example, a modest increase across all income tax brackets could generate substantial revenue. However, the political feasibility of significant tax hikes is questionable, particularly given the current cost of living crisis.
Public acceptance would likely be low, potentially leading to voter backlash and social unrest. A well-designed communication strategy would be crucial, emphasizing the necessity of the tax increases to safeguard the nation’s financial stability and outlining how the revenue will be used responsibly. The government might highlight investment in crucial public services like healthcare or infrastructure as a direct benefit resulting from the tax increase.
Spending Cuts
Alternatively, the government could reduce public spending to alleviate the fiscal burden. This could involve cuts to various government departments, potentially affecting public services such as healthcare, education, or social welfare programs. For instance, a reduction in departmental budgets by a certain percentage could lead to significant savings. The political implications are considerable, as cuts in public services are generally unpopular and could lead to protests and accusations of neglecting vital areas.
A successful communication strategy would need to carefully explain the necessity of the cuts, highlighting efficiency improvements and the avoidance of more drastic measures. Transparency in the allocation of remaining funds and a clear demonstration of how cuts were chosen based on impact would be essential to maintain public trust.
Debt Restructuring
Debt restructuring involves renegotiating the terms of existing government debt, potentially extending repayment periods or lowering interest rates. This could reduce the immediate pressure on government finances. However, this option carries risks. It could damage the UK’s credit rating, making future borrowing more expensive. For example, if the government were to negotiate longer repayment periods with its bondholders, this could lead to higher overall interest payments in the long term.
So, Britain’s facing a whopping £200bn loss from quantitative easing – how do we even begin to tackle that? It’s a massive economic headache, and honestly, makes me think about the bigger picture of international cooperation. The fact that europe is bidding a steady farewell to passport-free travel highlights how quickly things can change on a global scale, impacting trade and economic stability.
This just reinforces the need for a really smart, long-term strategy for managing those QE losses, to ensure Britain’s financial resilience in a rapidly changing world.
The political implications would be significant, as it might signal a lack of fiscal discipline and undermine confidence in the UK economy. A clear and detailed explanation of the restructuring process and its projected long-term impact would be essential to reassure the public and international investors.
International Comparisons and Best Practices
The UK’s predicament with QE losses isn’t unique. Many nations implemented similar large-scale asset purchase programs during and after the 2008 financial crisis and the recent pandemic, facing varying degrees of success and subsequent challenges. Examining how other countries have navigated these losses can offer valuable insights and potential solutions for the UK. By studying different approaches, the UK can learn from both successes and failures, tailoring a response that best suits its specific economic context.The scale of QE programs and the subsequent impact on government balance sheets varied significantly across countries.
Factors such as the size of the initial program, the maturity of the assets purchased, and the prevailing interest rate environment all played a crucial role in determining the ultimate financial consequences. Analyzing these factors alongside the responses adopted by different governments can provide a framework for evaluating potential UK strategies.
Comparison of QE Loss Management Strategies
Several countries faced substantial losses from their QE programs. A comparative analysis of their responses highlights diverse approaches and their relative effectiveness. The following Artikels three distinct strategies employed by different nations:
- Japan: Gradual unwinding and fiscal policy support. Japan’s approach involved a slow and gradual unwinding of its QE program, coupled with significant fiscal stimulus measures to offset the potential negative economic impacts. This strategy aimed to minimize market disruption while addressing the broader economic challenges. While effective in preventing a sudden shock, the long-term impact on Japan’s debt levels remains a subject of ongoing debate.
So, Britain’s facing a whopping £200bn loss from quantitative easing – how do we even begin to address that? It’s a massive financial headache, almost as perplexing as the recent trend I read about, the rise of the £40,000 gym membership , which shows how some people are spending their money. Perhaps finding solutions to the QE losses requires a similar level of creative financial thinking.
We need innovative solutions, not just austerity measures.
The slow unwinding minimized market volatility, but the fiscal stimulus added to the nation’s already substantial debt burden. This highlights the trade-off between market stability and long-term fiscal sustainability.
- United States: Targeted interventions and market monitoring. The US focused on targeted interventions in specific market segments rather than a blanket approach. This involved close monitoring of market conditions and adjusting their approach as needed. This strategy aimed to maximize the effectiveness of the interventions while minimizing the overall risk. The flexibility of this approach allowed for adaptation to changing economic circumstances, but it also required significant expertise and resources for effective market monitoring and intervention.
The successful navigation of the 2008 crisis demonstrates the potential of this approach, but it also requires a sophisticated understanding of market dynamics.
- Switzerland: Asset sales and diversification. Switzerland pursued a strategy of diversifying its holdings and gradually selling off assets to offset losses. This strategy aimed to minimize the impact on the government’s balance sheet while maximizing returns from asset sales. This approach requires careful timing and market analysis to ensure optimal sales prices. The success of this approach depends on market conditions and the ability to predict future interest rate movements accurately.
While this approach potentially reduces the overall burden, it might also impact market liquidity and stability if not implemented cautiously.
Risk Management and Contingency Planning
Addressing the £200 billion quantitative easing (QE) losses requires a robust risk management framework. Failure to adequately plan for potential negative consequences could exacerbate economic instability and erode public trust in the government’s financial stewardship. This section Artikels key risks, a contingency plan, and a monitoring procedure.
Key Risks Associated with Policy Options
The choice of policy to address the QE losses presents several distinct risks. For instance, a policy focusing on gradual repayment through increased taxation might lead to reduced consumer spending and stifle economic growth, potentially triggering a recession. Conversely, a policy of writing off the losses, while seemingly simpler, could damage the credibility of the Bank of England and potentially inflate future borrowing costs.
Finally, monetizing the losses by printing more money carries the significant risk of accelerating inflation, eroding the purchasing power of citizens and potentially leading to social unrest. Each approach demands careful consideration of its potential downsides.
Contingency Plan for Unforeseen Economic Shocks
A comprehensive contingency plan is crucial to mitigate the impact of unforeseen economic shocks resulting from QE loss management. This plan should include:
- Early Warning System: Establishing a sophisticated system to monitor key economic indicators (inflation, unemployment, GDP growth, consumer confidence) for early signs of distress. This might involve utilising advanced econometric modelling and scenario planning to predict potential crises before they fully manifest.
- Fiscal Reserve: Setting aside a significant fiscal reserve—perhaps a percentage of GDP—to act as a buffer against negative economic shocks. This reserve could be used to fund targeted fiscal stimulus measures (e.g., tax cuts, increased welfare spending) should a recession occur.
- Monetary Policy Flexibility: Granting the Bank of England greater flexibility in its monetary policy response. This might involve allowing for more aggressive interest rate cuts or quantitative easing measures if needed to stimulate the economy.
- International Cooperation: Strengthening international cooperation with other central banks and financial institutions to coordinate responses to global economic shocks. This collaborative approach would ensure a unified front against potential economic downturns.
For example, the 2008 financial crisis highlighted the need for swift and decisive action. A well-funded fiscal reserve and the ability to rapidly adjust monetary policy were crucial in mitigating the severity of the downturn in many countries.
Procedure for Monitoring and Managing Risks
Effective risk management requires a structured approach. The government should:
- Regular Risk Assessments: Conduct regular (e.g., quarterly) assessments of the risks associated with the chosen policy, considering both economic and political factors. This ongoing evaluation should incorporate expert opinion and data analysis.
- Transparent Reporting: Publish transparent and comprehensive reports on the QE losses, the chosen policy, and the effectiveness of risk management measures. This open communication builds public trust and ensures accountability.
- Adaptive Strategy: Develop an adaptive strategy that allows for adjustments to the chosen policy based on the evolving economic landscape and risk assessments. This flexibility is essential to navigate unexpected challenges effectively.
- Independent Oversight: Establish an independent body to oversee the risk management process and provide objective evaluations of its effectiveness. This ensures that the government’s actions are scrutinized and that any shortcomings are identified and addressed promptly.
A similar approach was adopted by the US Federal Reserve during the 2008 crisis, with regular stress tests and transparent communication playing a crucial role in restoring confidence in the financial system.
Impact on Financial Markets and the City of London
The £200 billion in quantitative easing (QE) losses represent a significant challenge for the UK, with potential ramifications extending far beyond the immediate budgetary implications. The impact on financial markets and the City of London’s standing as a global financial hub is a critical area requiring careful consideration. The scale of these losses and the uncertainty surrounding their handling could erode confidence in the UK’s financial stability, potentially triggering a cascade of negative consequences.The potential for market instability stems from several factors.
Firstly, the sheer size of the losses could lead to a reassessment of UK sovereign debt risk, potentially increasing borrowing costs for the government and the private sector. This increased cost of borrowing could stifle economic growth and negatively impact investment. Secondly, the uncertainty surrounding the government’s strategy to address these losses could create volatility in the markets, as investors grapple with the unknown.
This uncertainty could lead to capital flight, as investors seek safer havens for their assets. Finally, a loss of confidence in the UK’s financial management could negatively affect the pound sterling, further impacting the cost of imports and potentially fueling inflation.
Consequences for the City of London
The City of London’s position as a global financial centre is intrinsically linked to the perceived stability and reliability of the UK’s financial system. The QE losses, and the government’s response to them, could significantly impact its reputation. A perceived weakening of the UK’s financial strength could lead to a decline in foreign investment, potentially causing job losses and a reduction in the City’s overall economic activity.
This could also impact the attractiveness of London as a location for financial firms, potentially leading to relocation of operations to other financial hubs. The ripple effects could be substantial, impacting related industries and contributing to a broader economic slowdown.
Maintaining Confidence in the UK Financial System
To mitigate these risks, the government needs to adopt a transparent and credible strategy to address the QE losses. This strategy should prioritize clear communication with financial markets and the public, outlining the government’s plan for managing the losses and minimizing their impact on the economy. Demonstrating a commitment to fiscal responsibility and sound financial management is crucial.
This could involve detailed explanations of the government’s approach, outlining the rationale behind its choices and addressing any concerns raised by stakeholders. Furthermore, the government should actively engage with international financial institutions and rating agencies to maintain a positive outlook on the UK’s financial standing. Building confidence requires proactive measures to reassure investors and maintain the UK’s reputation as a stable and reliable financial partner.
The government’s ability to effectively manage this situation will be a key determinant of the UK’s future economic prosperity.
The £200bn loss from quantitative easing presents a significant challenge to Britain’s economic future. There’s no easy answer, and any chosen path will involve difficult decisions and potential trade-offs. However, by carefully considering the various policy options, their potential short-term and long-term impacts, and learning from international experiences, the UK can develop a robust and responsible strategy to manage this situation.
Transparency and open communication with the public will be crucial throughout this process. Ultimately, the success of any approach will depend on its ability to balance fiscal responsibility with the need to maintain economic stability and protect vital public services. This is a conversation that needs to continue, involving economists, policymakers, and the public alike.