Progress on the Science of Menstruation at Last
Progress on the science of menstruation at last! For centuries, menstruation has been shrouded in mystery, misinformation, and even stigma. But thankfully, we’re finally seeing a significant shift. Recent breakthroughs are illuminating the complex hormonal dance of our cycles, revealing the intricacies of menstrual disorders, and challenging outdated cultural beliefs. This journey into the fascinating world of menstruation will explore the latest scientific advancements, debunk common myths, and highlight the ongoing fight for better menstrual health worldwide.
From the historical context of menstruation research, marked by both progress and prejudice, to the exciting frontiers of current research employing AI and big data, we’ll delve into the science, the social impact, and the future of menstrual health. We’ll cover everything from understanding the hormonal processes driving our cycles to addressing common disorders like PMS and endometriosis, and even exploring the global disparities in access to menstrual hygiene products.
Get ready for an enlightening exploration of a topic that impacts half the world’s population.
Historical Context of Menstruation Research
For centuries, menstruation has been shrouded in mystery, fear, and misinformation. Scientific understanding of this fundamental biological process has evolved dramatically, moving from superstition and taboo to sophisticated investigation of its intricate mechanisms. This journey reflects not only advances in medical science but also shifting societal attitudes towards women’s health and bodies.The historical perspective on menstruation reveals a fascinating interplay between scientific progress and cultural biases.
Early civilizations often viewed menstruation with a mix of awe and apprehension, associating it with supernatural powers, impurity, or even disease. These beliefs heavily influenced societal practices and shaped the limited research conducted on the subject.
Early Misconceptions and Cultural Influences
Early medical texts often portrayed menstruation as a debilitating condition requiring restrictive practices. Ancient Greek physicians, for instance, linked menstruation to the imbalance of bodily humors, a theory that persisted for centuries. These beliefs often led to restrictive practices for menstruating women, isolating them from society or limiting their participation in daily life. Cultural taboos varied widely across different societies, sometimes involving ritualistic purification ceremonies or dietary restrictions.
The lack of open discussion and the stigma surrounding menstruation significantly hindered scientific inquiry. These cultural barriers directly impacted the type and quality of research undertaken. For example, the focus remained on managing perceived negative symptoms rather than understanding the underlying physiological processes.
Key Milestones in Menstrual Research
The scientific study of menstruation gained momentum during the 19th and 20th centuries with advancements in microscopy and physiology. The discovery of the ovarian cycle and the hormonal regulation of menstruation marked a significant turning point. Researchers like Edgar Allen and Edward Doisy’s identification of estrogen in the 1920s was a pivotal breakthrough, providing a crucial piece of the puzzle in understanding the hormonal control of menstruation.
Subsequent research illuminated the roles of other hormones like progesterone and the intricate interplay between the hypothalamus, pituitary gland, and ovaries. The development of effective contraception, such as the birth control pill, further advanced our understanding of the menstrual cycle and its hormonal regulation. The invention of techniques like ultrasound and hormone assays allowed for non-invasive and precise monitoring of the menstrual cycle, furthering research possibilities.
Comparison of Early and Current Understanding
Early beliefs about menstruation often lacked a biological basis, attributing the process to mystical forces or humoral imbalances. Current scientific knowledge emphasizes the complex interplay of hormones, specifically estrogen and progesterone, in regulating the uterine lining’s growth and shedding. While early explanations focused on perceived negative consequences, modern science recognizes menstruation as a normal physiological process integral to reproductive health.
The shift from viewing menstruation as a disease or a sign of impurity to understanding it as a natural and cyclical event is a testament to the progress made in both scientific understanding and societal attitudes. For example, the once-prevalent notion that menstruation caused illness or weakened women is now widely refuted by scientific evidence.
Societal and Cultural Influences on Research, Progress on the science of menstruation at last
The societal and cultural context has significantly shaped the direction and pace of menstrual research. The historical marginalization of women in science and medicine has undeniably limited research focused on female reproductive health. However, the growing awareness of gender inequality in research and the increased advocacy for women’s health have led to a surge in research on menstruation-related issues, including menstrual disorders like endometriosis and premenstrual syndrome (PMS).
The ongoing research is increasingly focusing on the broader impacts of menstruation on women’s overall health and well-being, reflecting a more holistic and inclusive approach. For instance, studies now explore the link between menstruation and mental health, chronic pain, and other health conditions.
Advances in Understanding Menstrual Physiology
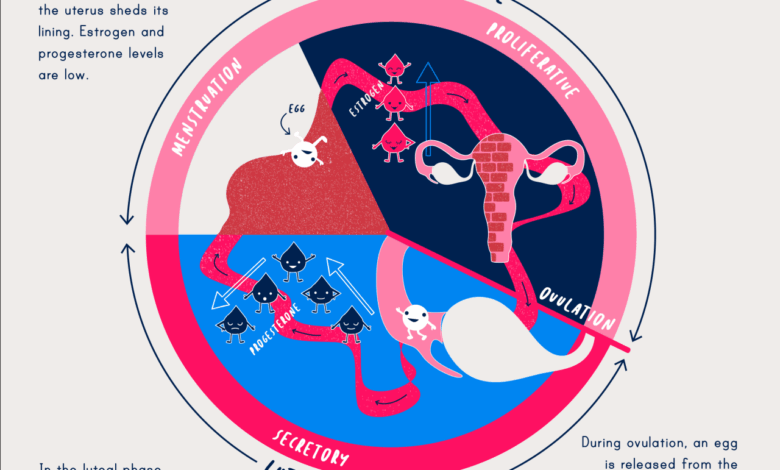
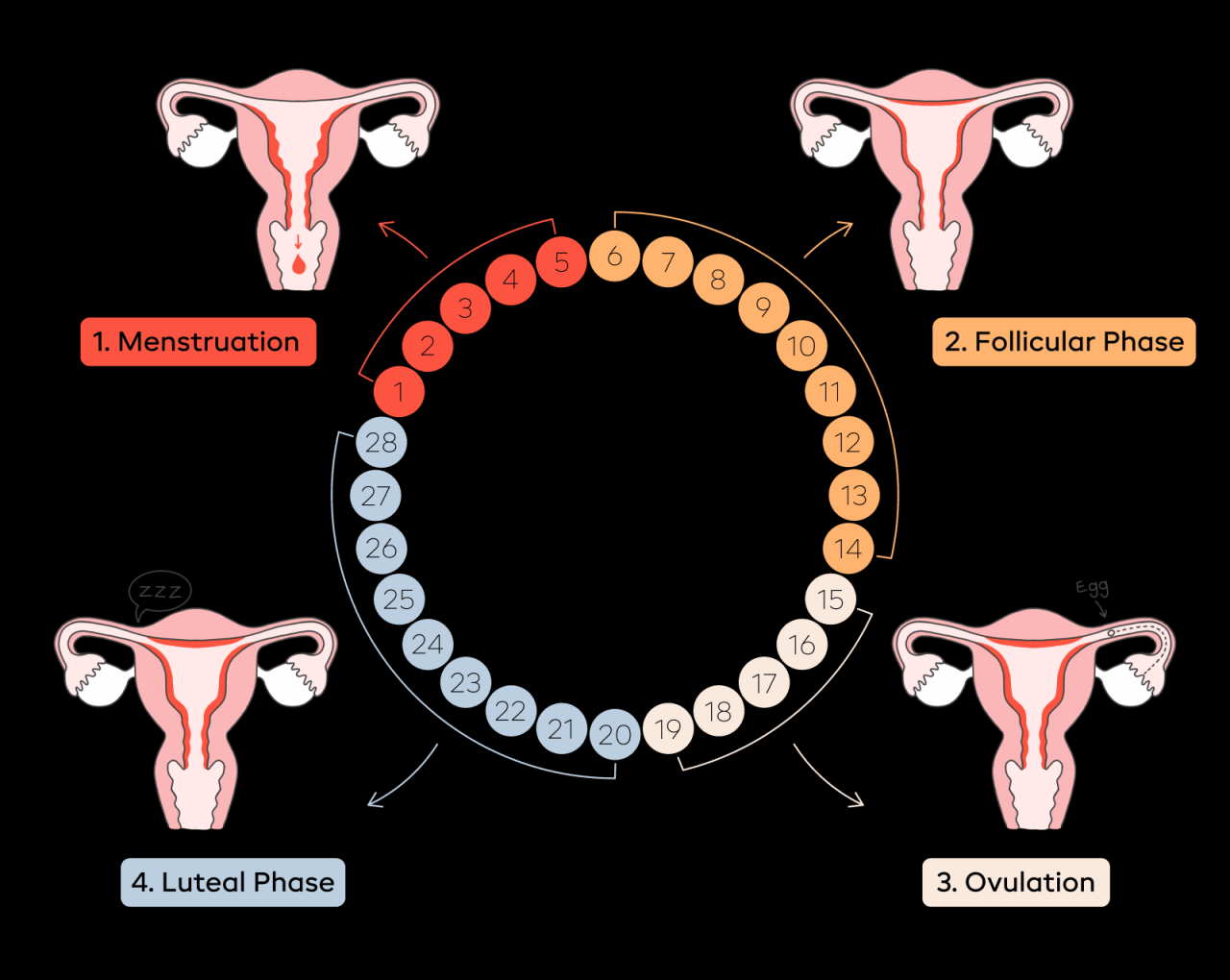
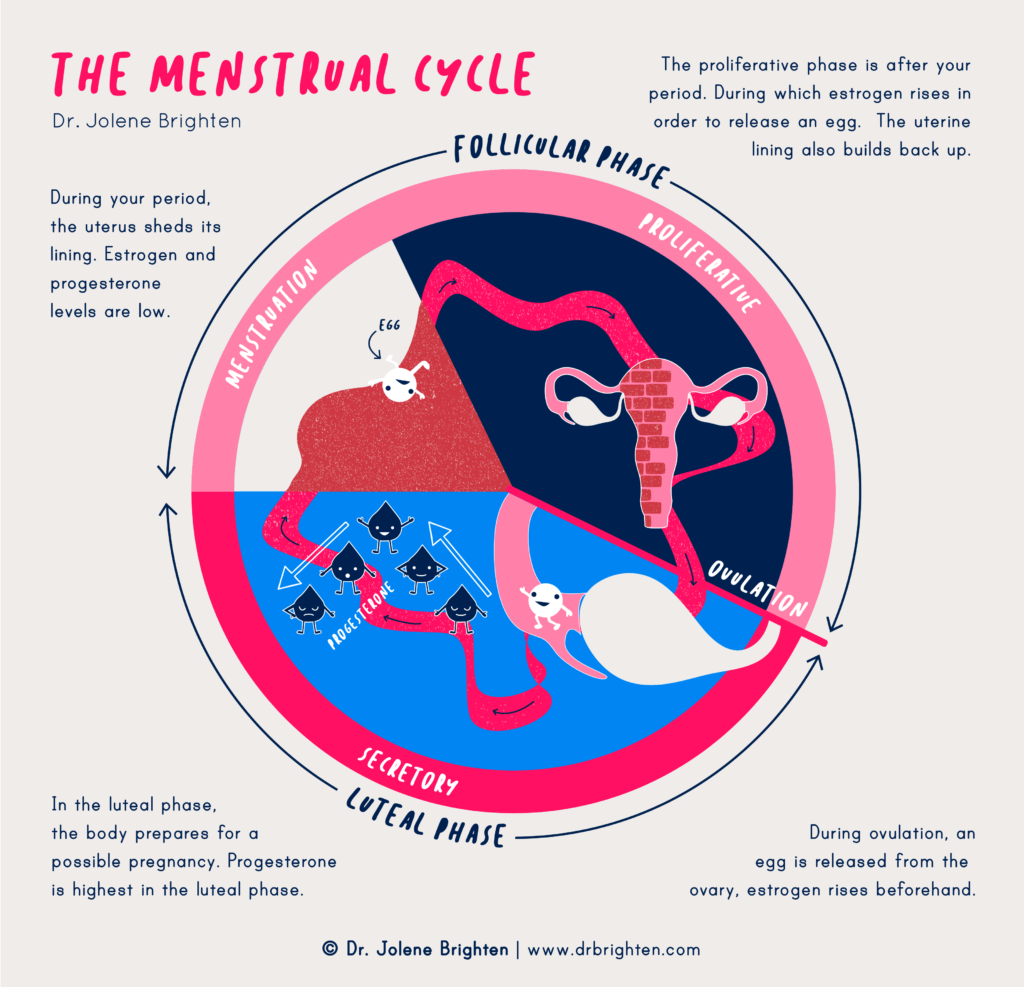
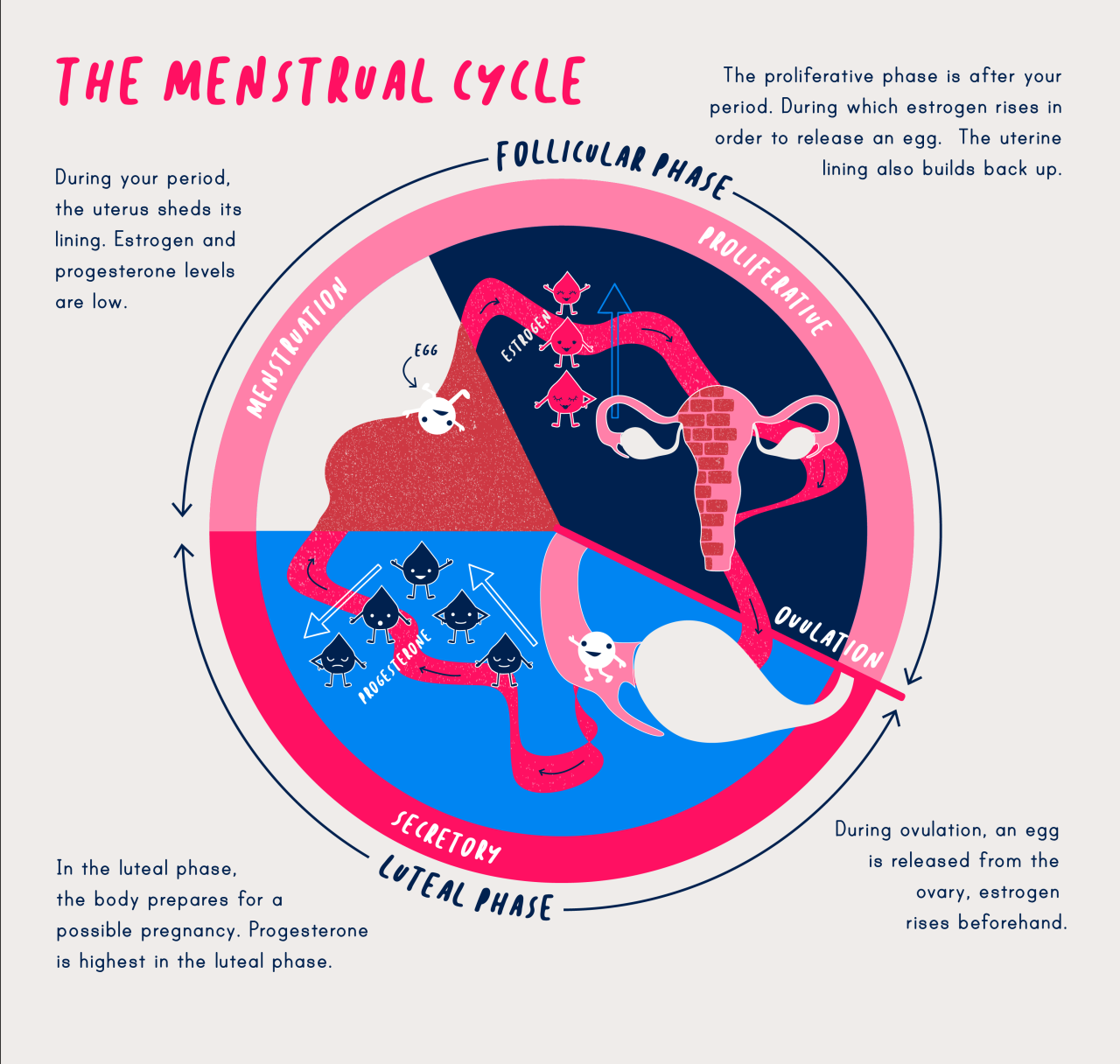
For centuries, menstruation was shrouded in mystery and misconception. However, significant advances in scientific understanding have revolutionized our comprehension of this complex physiological process. This improved understanding has not only dispelled harmful myths but also paved the way for better diagnostics, treatments, and overall reproductive health management.The menstrual cycle is a finely orchestrated interplay of hormones, resulting in the cyclical preparation of the uterus for potential pregnancy.
Failure of fertilization initiates the shedding of the uterine lining, leading to menstruation. This intricate process involves a complex feedback loop between the brain, ovaries, and uterus.
Hormonal Regulation of the Menstrual Cycle
The menstrual cycle is primarily governed by the intricate dance of several key hormones. The hypothalamus, a region of the brain, releases gonadotropin-releasing hormone (GnRH), which stimulates the pituitary gland to produce follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH triggers the maturation of ovarian follicles, each containing an egg. Simultaneously, these developing follicles begin producing estrogen, which causes the uterine lining (endometrium) to thicken and prepare for a potential pregnancy.
A surge in LH triggers ovulation, the release of the mature egg from the follicle. The ruptured follicle then transforms into the corpus luteum, which produces progesterone. Progesterone further thickens the endometrium, making it receptive to a fertilized egg. If fertilization doesn’t occur, the corpus luteum degenerates, leading to a drop in progesterone and estrogen levels, initiating menstruation.
Endometrial Changes Throughout the Menstrual Cycle
The endometrium, the inner lining of the uterus, undergoes dramatic cyclical changes throughout the menstrual cycle. Under the influence of estrogen and progesterone, the endometrium proliferates (thickens) during the follicular phase (before ovulation) and then enters the secretory phase (after ovulation) where it becomes highly vascularized and prepared for implantation of a fertilized egg. If implantation doesn’t occur, the endometrium breaks down and sheds, resulting in menstrual bleeding.
This process involves the breakdown of blood vessels and tissue, causing the characteristic bleeding associated with menstruation. The extent of endometrial thickening and the subsequent shedding can vary significantly between individuals.
Physiological Mechanisms of Menstrual Bleeding
Menstrual bleeding is a result of the breakdown of the endometrium, a process involving complex physiological mechanisms. The decrease in progesterone and estrogen levels triggers the spiral arteries in the endometrium to constrict, reducing blood flow. This ischemia (lack of blood supply) leads to tissue necrosis (cell death) and ultimately the shedding of the endometrial lining. The breakdown of tissue and blood vessels releases blood, tissue fragments, and other substances, which are expelled from the body through the vagina.
The duration and amount of bleeding vary considerably among individuals, and factors such as stress, diet, and genetics can influence these variations. The process is tightly regulated to ensure the integrity of the uterine lining is maintained between cycles, preventing excessive bleeding or other complications.
Menstrual Disorders and Treatments
Understanding and managing menstrual disorders is crucial for the well-being of countless individuals. These conditions can significantly impact daily life, causing pain, discomfort, and emotional distress. Fortunately, advancements in medical research have led to a broader understanding of their causes and more effective treatment options.
Common Menstrual Disorders
Several common menstrual disorders affect women of reproductive age. These include premenstrual syndrome (PMS), endometriosis, and polycystic ovary syndrome (PCOS). Each condition presents with a unique set of symptoms, requiring specific diagnostic approaches and tailored treatment strategies.
Premenstrual Syndrome (PMS)
PMS is characterized by a range of physical and emotional symptoms that occur in the luteal phase of the menstrual cycle, typically the week or two before menstruation. Symptoms can vary widely among individuals but commonly include bloating, breast tenderness, mood swings, irritability, fatigue, and headaches. Diagnosis is primarily based on symptom tracking and exclusion of other conditions. Treatment options range from lifestyle modifications (diet, exercise, stress management) to over-the-counter pain relievers and, in severe cases, prescription medications like selective serotonin reuptake inhibitors (SSRIs) or birth control pills.
The effectiveness of treatment depends on the severity of symptoms and individual response. Side effects of medications can include nausea, weight gain, or changes in libido.
Endometriosis
Endometriosis involves the growth of endometrial-like tissue outside the uterus. This misplaced tissue responds to hormonal changes, leading to inflammation, pain, and potentially infertility. Symptoms often include chronic pelvic pain, heavy menstrual bleeding, painful intercourse (dyspareunia), and infertility. Diagnosis typically involves a pelvic exam, ultrasound, and sometimes laparoscopy, a minimally invasive surgical procedure to visualize and biopsy the affected tissue.
Treatment options include pain management with NSAIDs or hormonal therapies (such as GnRH agonists or progestins), surgery to remove endometrial implants, and in some cases, assisted reproductive technologies (ART). Side effects of hormonal therapies can include hot flashes, vaginal dryness, and mood changes. Surgical interventions carry risks associated with any surgical procedure.
Polycystic Ovary Syndrome (PCOS)
PCOS is a hormonal disorder characterized by irregular periods, elevated androgen levels, and the development of cysts on the ovaries. Symptoms can include irregular or absent menstruation, acne, excessive hair growth (hirsutism), weight gain, and infertility. Diagnosis involves clinical evaluation, blood tests to assess hormone levels, and ultrasound to visualize the ovaries. Treatment focuses on managing symptoms and improving fertility.
It’s amazing to see the leaps and bounds in menstrual health research; finally, we’re getting the science-backed solutions we deserve! It makes me think about data security, though – the news about the election software CEO arrested over data theft storing data on servers in China highlights how vulnerable sensitive information can be. Hopefully, the same level of technological advancement will protect our health data as well, ensuring that progress in menstrual health research benefits everyone safely.
Options include lifestyle modifications (weight loss, diet, exercise), oral contraceptives to regulate periods, medications to reduce androgen levels, and fertility treatments if pregnancy is desired. Side effects of medications can vary depending on the specific drug but may include weight changes, mood swings, or increased risk of blood clots.
Treatment Comparison for Endometriosis
| Treatment | Description | Effectiveness | Potential Side Effects |
|---|---|---|---|
| Medication (Hormonal Therapy) | GnRH agonists, progestins, oral contraceptives; aim to suppress endometrial growth. | Variable; effective for pain management in many, but may not address underlying condition. | Hot flashes, vaginal dryness, weight gain, mood changes, decreased bone density (long-term use). |
| Surgery (Laparoscopic or Open) | Removal of endometrial implants; may involve ablation or excision. | Can provide significant pain relief and improve fertility; effectiveness depends on extent of disease. | Surgical risks (infection, bleeding, scarring), potential for recurrence. |
| Alternative Therapies | Acupuncture, herbal remedies; often used in conjunction with conventional treatments. | Limited scientific evidence of effectiveness; may provide some pain relief for some individuals. | Potential for interactions with other medications; variable quality control of herbal products. |
Menstrual Hygiene and Public Health
Menstruation, a fundamental biological process, is often shrouded in stigma and misinformation, particularly in low-resource settings. Access to proper menstrual hygiene management (MHM) is not merely a matter of comfort; it’s a critical public health issue directly impacting the health, education, and economic empowerment of women and girls globally. The lack of access to safe and hygienic products and information creates significant disparities and detrimental health consequences.Global Disparities in Menstrual Hygiene Access and EducationAccess to menstrual hygiene products and education varies drastically across the globe.
In many low-income countries, poverty, cultural norms, and lack of infrastructure create significant barriers. Girls and women may lack access to clean water, sanitation facilities, and affordable sanitary products. Furthermore, limited education surrounding menstruation perpetuates harmful myths and practices, leading to increased health risks and social exclusion. For instance, in some regions, girls miss school during their periods, impacting their educational attainment and future opportunities.
This disparity is not merely a geographical issue; it also exists within countries, particularly between rural and urban populations.Impact of Poor Menstrual Hygiene on Women’s Health and Well-beingPoor menstrual hygiene practices significantly impact women’s health and well-being. The use of unsanitary materials, such as rags or leaves, increases the risk of infections like urinary tract infections (UTIs), reproductive tract infections (RTIs), and other gynecological problems.
These infections can lead to chronic health issues, infertility, and even death. The stigma associated with menstruation often prevents women from seeking medical care when experiencing problems, further exacerbating the situation. Furthermore, the financial burden of purchasing sanitary products can be substantial for low-income families, forcing many to compromise on hygiene, potentially resulting in severe health consequences.
The psychological impact of managing menstruation unsafely, combined with the social stigma, can lead to significant stress and anxiety.Best Practices for Menstrual Hygiene ManagementBest practices for MHM involve several key elements. Firstly, access to affordable, safe, and absorbent menstrual products is crucial. Secondly, access to clean water and sanitation facilities for disposal is equally important. Thirdly, comprehensive education on menstrual health, including hygiene practices and myth-busting, is vital.
This education should be age-appropriate and culturally sensitive, empowering girls and women to manage their menstruation safely and confidently. Furthermore, promoting open conversations about menstruation helps to reduce stigma and encourages help-seeking behavior. Finally, governments and organizations need to implement policies and programs that support MHM, including subsidies for menstrual products and investment in sanitation infrastructure.Effectiveness of Different Menstrual Hygiene ProductsThe effectiveness of different menstrual hygiene products depends on several factors, including individual needs and preferences, cost, availability, and environmental impact.
- Pads: Widely available and relatively inexpensive, but can be bulky, less comfortable, and generate significant waste.
- Tampons: Convenient and discreet, but can cause toxic shock syndrome (TSS) if used improperly and generate significant waste.
- Menstrual Cups: Reusable, environmentally friendly, and cost-effective in the long run, but require proper insertion and cleaning techniques. They may not be suitable for all individuals.
- Menstrual Discs: Similar to cups, but sit lower in the vagina. They may also require a learning curve for insertion and removal.
- Menstrual Underwear: Absorbent underwear that can be worn instead of other products. They can be comfortable and discreet but can be expensive and require specific washing instructions.
A Public Health Campaign for Improved Menstrual Hygiene in a Low-Resource SettingA successful public health campaign in a low-resource setting would need a multi-pronged approach. The campaign, titled “Periods with Dignity,” would focus on:
1. Education and Awareness
School-based programs would teach girls about menstruation, dispelling myths and promoting proper hygiene practices. Community-based workshops would engage women and their families, emphasizing the importance of MHM. Materials would be culturally appropriate and use local languages.
2. Access to Products
Subsidized or free distribution of reusable menstrual products, such as cloth pads or menstrual cups, would be implemented. Training on proper use and cleaning would be provided.
3. Improved Sanitation
Advocacy for improved sanitation infrastructure in schools and communities would be undertaken, including the construction of clean and private latrines with handwashing facilities.
4. Community Engagement
It’s amazing to finally see real progress on the science of menstruation, with more research focusing on the complexities of the female body. However, we need to consider the broader health picture; a recent reanalysis of vaccine trial data, found in this study vaccinated at higher risk of serious adverse events reanalysis of original trial data , highlights the need for comprehensive research across all health areas.
Understanding these potential side effects is crucial for ensuring holistic women’s health, allowing us to better understand the interplay between vaccination and menstrual health.
Working with community leaders and influencers to challenge stigma and promote open dialogue about menstruation would be crucial.
5. Sustainability
The campaign would focus on sustainable solutions, including training women on making reusable pads and promoting environmentally friendly disposal methods.The success of the campaign would be measured through indicators such as school attendance rates among menstruating girls, the prevalence of menstrual-related infections, and community awareness levels. Regular monitoring and evaluation would be essential to adapt strategies and ensure the campaign’s effectiveness.
A successful campaign would ultimately empower women and girls, improving their health, education, and overall well-being.
Menstruation and Reproductive Health: Progress On The Science Of Menstruation At Last
Menstruation is intrinsically linked to reproductive health, serving as a key indicator of overall well-being and fertility. Understanding the nuances of this relationship is crucial for women’s health management and family planning. The regular menstrual cycle reflects the intricate interplay of hormones and physiological processes essential for conception and pregnancy. Disruptions to this cycle can signal underlying health issues, impacting reproductive potential.
Finally, we’re seeing real progress on the science of menstruation, with more research funding and less stigma. It’s a stark contrast to some of the bizarre news out there, like the fact that, believe it or not, turkey wants the EU to regulate the doner kebab. Seriously, who knew? But back to the important stuff – the increased understanding of menstrual health is truly groundbreaking and long overdue.
Menstruation and Fertility
The menstrual cycle is the foundation of female fertility. The regular shedding of the uterine lining (menstruation) occurs when pregnancy doesn’t occur. The fertile window, the period when conception is most likely, typically falls within the days leading up to and including ovulation, which usually occurs around 12-16 days before the next menstrual period. Hormonal changes throughout the cycle—the rise in estrogen followed by a surge in luteinizing hormone (LH) triggering ovulation—are critical for egg release and the preparation of the uterus for implantation.
Consistent, regular cycles suggest a healthy hormonal balance, increasing the likelihood of conception. Conversely, irregular cycles can indicate hormonal imbalances that may affect fertility.
Menstrual Cycle Tracking for Family Planning
Tracking the menstrual cycle is a fundamental aspect of natural family planning methods. By meticulously recording the length of cycles and noting symptoms like changes in cervical mucus and basal body temperature, women can identify their fertile window and use this information to either avoid or plan pregnancy. Mobile apps and calendar-based methods assist in tracking and predicting ovulation.
For example, a woman with consistently 28-day cycles might anticipate her fertile window between days 10 and 18. However, it’s important to note that this method is not foolproof, and other methods of contraception may be needed for reliable family planning.
Impact of Menstrual Irregularities on Reproductive Health
Irregular or absent menstruation (amenorrhea) can signify various underlying health conditions, many of which can impact fertility. These include polycystic ovary syndrome (PCOS), thyroid disorders, hormonal imbalances, and even significant stress. PCOS, for example, is characterized by irregular periods, high levels of androgens, and ovarian cysts, significantly reducing fertility. Similarly, conditions affecting the hypothalamus or pituitary gland, which regulate hormonal production, can disrupt the menstrual cycle and impact reproductive potential.
Early diagnosis and treatment of these conditions are vital to improve reproductive health outcomes.
Menstruation and Other Aspects of Women’s Health
The menstrual cycle influences various aspects of women’s health beyond fertility. Hormonal fluctuations during the cycle can affect mood, energy levels, and even cognitive function. Some women experience premenstrual syndrome (PMS), characterized by symptoms like bloating, mood swings, and breast tenderness. Severe PMS can significantly impact daily life. Additionally, the menstrual cycle is linked to the risk of certain health conditions, such as endometriosis and migraines.
Understanding the interplay between menstruation and overall health allows for proactive management of these conditions and improved well-being.
Emerging Research Areas in Menstruation Science
The field of menstruation research is experiencing a renaissance, fueled by advancements in technology and a growing recognition of the profound impact menstrual health has on overall well-being. We’re moving beyond simply managing symptoms to understanding the complex interplay of hormones, genetics, and the environment that shapes the menstrual experience. This is leading to exciting new avenues of investigation with the potential to revolutionize women’s healthcare.The application of new technologies and methodologies is accelerating progress at an unprecedented rate.
This allows for more precise measurements, larger datasets, and more sophisticated analyses, leading to a deeper understanding of the menstrual cycle and its associated conditions.
The Role of the Microbiome in Menstrual Health
The human microbiome, the vast community of microorganisms living in and on our bodies, is increasingly recognized as a crucial factor influencing health and disease. Research is actively exploring the composition and function of the vaginal and gut microbiomes during the menstrual cycle, investigating their roles in maintaining reproductive health and contributing to conditions like endometriosis and premenstrual syndrome (PMS).
Studies are focusing on identifying specific microbial signatures associated with different menstrual phases and health outcomes. For example, researchers are investigating whether certain bacterial strains might be protective against bacterial vaginosis, a common condition affecting many women during menstruation. This research holds the potential for developing novel microbiome-based therapies for improving menstrual health.
Artificial Intelligence and Big Data in Menstrual Cycle Analysis
AI and big data analytics are transforming the way we analyze menstrual cycle data. Wearable sensors and mobile apps are collecting vast amounts of information on menstrual bleeding patterns, cycle length, symptoms, and other physiological parameters. AI algorithms can analyze these data to identify patterns and predict individual risk for menstrual disorders. For instance, AI could be used to predict the onset of heavy bleeding in women with menorrhagia or to identify early warning signs of endometriosis.
The ability to personalize predictions based on individual data offers the potential for more effective prevention and management strategies. One example of this in action is the development of apps that track menstrual cycles and provide personalized insights and predictions. These apps are not only providing valuable data for researchers but also empowering women to better understand and manage their own menstrual health.
Ongoing Clinical Trials Targeting Menstrual Disorders
Several clinical trials are currently underway investigating novel treatments for menstrual disorders. These trials are exploring new pharmacological approaches, such as targeted hormone therapies and immunomodulatory agents, to address conditions like endometriosis, heavy menstrual bleeding, and PMS. For example, studies are exploring the efficacy of new drugs that selectively target the inflammatory pathways involved in endometriosis, potentially reducing pain and improving fertility outcomes.
These trials often involve large, diverse populations, allowing researchers to gain a more comprehensive understanding of the effectiveness and safety of these new treatments across various demographics. The results of these trials will play a crucial role in shaping future guidelines for the management of menstrual disorders.
The Impact on Women’s Health and Well-being
The advancements in menstruation science have the potential to significantly improve women’s health and well-being. By developing more effective diagnostic tools and treatments, we can reduce the burden of menstrual disorders, improve quality of life, and enhance reproductive health. This includes reducing missed work or school days due to menstrual symptoms, decreasing the need for invasive procedures, and improving overall health outcomes.
The ability to predict and personalize interventions also empowers women to take control of their own health and make informed decisions about their reproductive future. This holistic approach to menstrual health is crucial for achieving gender equality in healthcare and ensuring that women have access to the information and resources they need to thrive.
Menstruation and its Impact on Women’s Lives
Menstruation, a natural biological process, significantly impacts women’s lives across the globe, extending far beyond the purely physiological. The experience is deeply intertwined with social norms, cultural beliefs, and economic realities, often resulting in unequal access to resources and opportunities. This section explores the multifaceted ways menstruation shapes women’s lives, highlighting the pervasive stigma, its impact on education and employment, and its overall effect on quality of life.
We’ll also examine initiatives designed to address these challenges and promote menstrual equity.
Social and Cultural Stigma Surrounding Menstruation
The social and cultural stigma surrounding menstruation varies widely across different societies. In some cultures, menstruation is viewed as taboo, unclean, or even shameful, leading to social isolation and discrimination against menstruating women. These beliefs often stem from deeply ingrained cultural and religious practices. For example, in some communities, menstruating women are restricted from participating in religious ceremonies or social gatherings, or are separated from the rest of the family.
In other cultures, a more open and positive attitude towards menstruation exists, with celebrations and rituals marking this stage of life. This difference underscores the significant role of cultural context in shaping perceptions and experiences of menstruation. The resulting stigma can lead to feelings of shame, embarrassment, and anxiety among women, hindering their ability to openly discuss menstruation and seek necessary support.
Impact of Menstruation on Women’s Education and Employment
Menstruation can significantly impact a woman’s access to education and employment opportunities. The lack of access to sanitary products, safe and private sanitation facilities, and adequate menstrual hygiene education can lead to absenteeism from school and work. This is particularly true in low-income settings where the cost of sanitary products can be a significant burden for families. Girls may miss school days during their periods, leading to poor academic performance and increased dropout rates.
Similarly, women may miss work days, affecting their productivity and earning potential. This economic disadvantage perpetuates a cycle of poverty and inequality, impacting not only the individual woman but also her family and community. In many parts of the world, the absence of open dialogue about menstruation further exacerbates these issues.
Menstrual Health and Women’s Overall Quality of Life
Menstrual health is intrinsically linked to a woman’s overall well-being. Experiencing painful periods, heavy bleeding (menorrhagia), or other menstrual disorders can significantly impact a woman’s physical and emotional health. The pain associated with dysmenorrhea can be debilitating, affecting daily activities and productivity. Heavy bleeding can lead to anemia, fatigue, and other health complications. Furthermore, the social stigma surrounding menstruation can exacerbate these issues, leading to feelings of isolation, shame, and anxiety.
These factors can collectively diminish a woman’s quality of life, impacting her relationships, self-esteem, and overall mental health. Access to appropriate healthcare, education, and support systems is crucial for improving menstrual health and overall well-being.
Initiatives Aimed at Breaking Down Stigma and Improving Access to Menstrual Health Resources
Numerous initiatives are underway globally to address the challenges associated with menstruation. These initiatives focus on breaking down stigma, improving access to menstrual health resources, and promoting menstrual hygiene management. For example, many non-governmental organizations (NGOs) and social enterprises are working to provide affordable and accessible sanitary products to women and girls in low-income communities. Educational programs are being implemented to raise awareness about menstrual health and hygiene, challenging harmful cultural beliefs and promoting open conversations.
Government policies are being developed to ensure that girls and women have access to sanitary products and menstrual hygiene facilities in schools and workplaces.
“Menstruation is not a disease; it’s a natural process. It’s time to break the silence and stigma surrounding it.”
The journey through the progress made in understanding menstruation has been both enlightening and empowering. While significant strides have been made, the fight for comprehensive menstrual health is far from over. The need for increased research, improved access to healthcare, and the dismantling of persistent stigmas remains crucial. However, the scientific advancements we’ve explored offer a beacon of hope, promising a future where menstruation is viewed not as a source of shame or mystery, but as a natural and vital part of women’s health and well-being.
The ongoing conversation, fueled by scientific curiosity and a commitment to equity, ensures a healthier and more informed future for generations to come.

