Genomic Medicines $3M a Dose? How to Make Them Affordable
Genomic medicines can cost 3m a dose how to make them affordable – Genomic medicines can cost 3m a dose, how to make them affordable? That’s the million-dollar question, literally. The groundbreaking potential of these life-saving treatments is undeniable, but their astronomical price tags raise serious concerns about accessibility and equity. This post dives into the complex factors driving these exorbitant costs – from hefty R&D investments to pharmaceutical pricing strategies – and explores innovative solutions to bridge the affordability gap, ensuring these advancements benefit everyone, not just the privileged few.
We’ll examine the roles of governments, regulatory bodies, and the pharmaceutical industry itself in shaping the cost of genomic medicines. We’ll also look at promising alternative financing models, like risk-sharing agreements and value-based pricing, and discuss the potential for technological advancements to bring down production costs. Ultimately, we’ll explore how patient advocacy and increased public awareness can play a crucial role in making these vital treatments available to all who need them.
The High Cost of Genomic Medicines: Genomic Medicines Can Cost 3m A Dose How To Make Them Affordable
The astronomical price tag of some genomic medicines, reaching $3 million per dose, raises serious concerns about accessibility and affordability. This cost isn’t arbitrary; it’s the culmination of a complex interplay of factors, from the intricate research and development process to the unique challenges of manufacturing and delivering these highly personalized therapies. Understanding these contributing factors is crucial to finding solutions that make these life-saving treatments available to those who need them.
Research and Development Costs
The journey from initial research to market approval for a genomic medicine is exceptionally long and expensive. Years of pre-clinical research, involving extensive laboratory work, animal testing, and the development of sophisticated analytical tools, are required. This is followed by lengthy and rigorous clinical trials involving multiple phases, each demanding significant investment in participant recruitment, data collection, analysis, and monitoring.
The astronomical cost of genomic medicines – some reaching $3 million a dose – is a huge barrier to access. Predicting the impact of such high prices is tricky, kind of like how how wrong could Americas pollsters be when forecasting election outcomes? Getting these life-saving treatments to those who need them requires innovative solutions and transparent pricing models, so we can actually make a difference in people’s lives.
The failure rate of drug candidates is high, meaning that many costly projects ultimately yield no marketable product. The sheer complexity of developing personalized therapies, which often target specific genetic mutations, adds another layer of expense. For example, the development of CAR T-cell therapy, a type of genomic medicine, involved substantial investment in gene engineering techniques and manufacturing processes tailored to each patient’s unique genetic profile.
The cost of specialized equipment, skilled personnel (geneticists, bioinformaticians, clinicians), and intellectual property rights protection also contribute significantly to the overall R&D expenditure.
Three million dollars a dose for genomic medicine? It’s mind-boggling, especially when considering the vast unknowns, like whether life exists elsewhere, for example, could life exist on one of Jupiter’s moons ? That kind of discovery might lead to breakthroughs that could drastically reduce the cost of these life-saving treatments, making them accessible to everyone. We need to invest in both space exploration and affordable healthcare innovation.
Manufacturing and Delivery Challenges
Manufacturing genomic medicines presents unique challenges compared to traditional pharmaceuticals. These therapies are often produced on a small scale, using complex and highly specialized processes. The individualized nature of many genomic medicines necessitates customized manufacturing for each patient, significantly increasing the production cost per dose. The need for rigorous quality control and stringent regulatory compliance further adds to the expense.
Delivery and administration of these therapies can also be complex and expensive, often requiring specialized personnel and hospital infrastructure. For instance, some gene therapies necessitate highly specialized infusion centers and continuous monitoring during and after administration.
Pricing Compared to Other Advanced Therapies
Genomic medicines are not alone in commanding high prices. Other advanced therapies, such as cell-based therapies and some targeted cancer drugs, also carry significant costs. However, the price of genomic medicines often surpasses these other therapies, largely due to the complexity of their development and the individualized nature of their production. While the high cost of other advanced therapies is a concern, the even higher price point for genomic medicines presents a greater barrier to access.
The justification for these costs often hinges on the potential for long-term benefit, potentially curing a disease rather than merely managing symptoms, but this potential does not automatically translate into affordability.
Cost Comparison Table
The following table provides a hypothetical comparison of the cost of genomic medicines to traditional treatments for similar conditions. Note that actual costs vary widely depending on the specific therapy, location, and other factors. These figures are intended to illustrate the magnitude of the price difference.
| Condition | Traditional Treatment Cost (Annual Estimate) | Genomic Medicine Cost (Per Dose) | Notes |
|---|---|---|---|
| Specific Type of Cancer | $100,000 | $2,500,000 | Traditional treatment may require ongoing medication and hospital visits. Genomic medicine might offer a one-time cure. |
| Rare Genetic Disorder | $50,000 | $3,000,000 | Traditional treatment may focus on managing symptoms. Genomic medicine could potentially address the underlying genetic defect. |
| Inherited Blood Disorder | $75,000 | $1,500,000 | Traditional treatments might involve regular blood transfusions or other interventions. Genomic medicine might offer a more permanent solution. |
Accessibility and Equity Issues
The exorbitant cost of genomic medicines, potentially reaching $3 million per dose, creates a stark reality: access to these life-saving treatments is severely limited, raising profound concerns about accessibility and equity. This isn’t simply a matter of affordability for individuals; it’s a systemic issue with far-reaching consequences for healthcare systems and society as a whole.The high price of genomic medicines disproportionately impacts patient access, creating a significant barrier for many who could benefit.
This unequal access deepens existing health disparities and raises crucial ethical questions about the fair distribution of potentially life-saving therapies. The financial burden is not equally distributed, leading to disparities in healthcare outcomes.
Populations Disproportionately Affected
Individuals lacking adequate health insurance coverage, those living in poverty, and members of marginalized communities are particularly vulnerable to the high cost of genomic medicines. The uninsured or underinsured often face insurmountable financial obstacles, leaving them unable to afford even a fraction of the treatment cost. Similarly, individuals from low-income backgrounds may lack the financial resources or social support to access these expensive therapies, even if they have insurance.
This creates a scenario where the benefits of genomic medicine are concentrated among wealthier populations, exacerbating existing health inequalities. For example, a family struggling to afford basic necessities would find the cost of a $3 million treatment utterly prohibitive, regardless of insurance status.
Ethical Considerations Surrounding Equitable Access
The ethical implications of unequal access to life-saving therapies are significant. The principle of justice demands equitable distribution of healthcare resources, regardless of socioeconomic status or other demographic factors. Denying access to potentially life-saving treatment based solely on financial constraints raises profound ethical concerns about fairness, justice, and the right to healthcare. This is especially critical for genomic medicines that may offer the only hope for individuals with rare or life-threatening conditions.
The question of who bears the responsibility for ensuring equitable access—governments, pharmaceutical companies, or individuals—is a complex one with no easy answers.
A Potential Tiered Pricing Model
One potential approach to improving access for low-income patients is a tiered pricing model. This model could involve setting different price points based on a patient’s ability to pay, determined through a comprehensive assessment of their financial resources and insurance coverage. For instance, the government or a philanthropic organization could subsidize a portion of the cost for low-income individuals, while those with greater financial capacity would pay a higher price.
This model would require a robust and transparent system for assessing financial need and ensuring equitable distribution of subsidies. A similar approach is already used in some countries for certain medications, with varying levels of success. The key to success would lie in designing a system that is both fair and efficient, avoiding undue administrative burden and preventing fraud.
Governmental and Regulatory Roles
The exorbitant cost of genomic medicines presents a significant challenge to healthcare systems worldwide. Addressing this requires a multifaceted approach, with governments and regulatory bodies playing a crucial role in shaping accessibility and affordability. Their interventions, ranging from direct price controls to incentivizing competition, can significantly impact the availability and cost of these life-saving treatments.Government policies aimed at controlling drug prices vary widely across nations, reflecting differing healthcare philosophies and economic priorities.
These policies often involve a complex interplay of market forces and governmental oversight, aiming to balance the need for pharmaceutical innovation with the imperative of ensuring patient access. The effectiveness of these policies is often debated, with arguments focusing on the potential impact on pharmaceutical research and development versus the need for affordable healthcare.
Examples of Government Policies Aimed at Controlling Drug Prices
Several countries employ different strategies to regulate pharmaceutical prices. For instance, the United States relies primarily on market-based mechanisms, supplemented by negotiated prices for Medicare Part D. In contrast, many European countries utilize reference pricing, where the price of a drug is set relative to similar medications in other countries. Canada employs a system of price negotiation and regulation, resulting in generally lower drug prices than in the US.
Three million dollars a dose? Genomic medicines are groundbreaking, but their price tag is insane. We need innovative solutions, and maybe we can learn from past mistakes; check out this article on lessons from Justin Trudeau’s failings in Canada for insights into effective (and ineffective) government healthcare strategies. Applying those lessons could be crucial in making these life-saving treatments accessible to everyone, not just the wealthy.
Australia utilizes a Pharmaceutical Benefits Scheme (PBS) which subsidizes the cost of many medications, making them more affordable to patients. These diverse approaches highlight the complex and varied landscape of pharmaceutical price regulation.
Comparison of Drug Pricing Regulations Across Different Countries, Genomic medicines can cost 3m a dose how to make them affordable
A comparison reveals stark differences. The United States generally has the highest drug prices globally, largely due to its reliance on a free market system and the lack of direct price negotiation for many drugs. European countries, on the other hand, often have significantly lower prices due to their various price control mechanisms. These include government-set prices, reference pricing, and parallel importing (where cheaper drugs from other countries are imported).
The price differences are often substantial, illustrating the impact of regulatory choices on drug affordability. For example, a cancer drug costing $10,000 in the US might cost $5,000 in Canada and even less in some European countries.
The Role of Regulatory Bodies in Approving and Pricing New Genomic Medicines
Regulatory bodies like the FDA (United States) and the EMA (European Medicines Agency) play a critical role in approving new genomic medicines. Their approval processes involve rigorous evaluation of safety and efficacy, influencing the time it takes for a new drug to reach the market. Pricing decisions, however, often involve a separate process, which may include negotiation with pharmaceutical companies, reference pricing, or other mechanisms.
The interaction between approval and pricing processes is complex and influences both the speed of access and the overall cost of new treatments. A faster approval process might not translate to lower prices, highlighting the need for coordinated policies addressing both aspects.
Potential Government Interventions to Reduce the Cost of Genomic Medicines
Several potential government interventions could reduce the cost of genomic medicines. These include: direct price negotiation with pharmaceutical companies; expanding government-sponsored insurance programs to cover a wider range of genomic medicines; incentivizing the development of biosimilars and generics; fostering competition among pharmaceutical companies; investing in research and development of more affordable genomic medicines; implementing policies that promote transparency in drug pricing; and exploring the use of value-based pricing models which link reimbursement to clinical outcomes.
Each of these strategies requires careful consideration of potential trade-offs, but they represent important tools for policymakers to explore.
Pharmaceutical Industry Practices
The astronomical cost of genomic medicines, often exceeding $3 million per dose, is a complex issue deeply intertwined with the pricing strategies of pharmaceutical companies. Understanding these strategies is crucial to addressing the accessibility and equity concerns surrounding these life-saving treatments. Profit margins, research and development costs, market demand, and patent protection all play significant roles in shaping the final price tag.The pricing strategies employed by pharmaceutical companies for genomic medicines are multifaceted and often criticized for prioritizing profit maximization over patient access.
Companies typically conduct extensive market research to determine the potential demand and the price patients or insurance providers are willing to pay. This analysis, combined with the high R&D costs associated with developing these complex therapies, justifies, in their view, the high price point. However, the lack of transparency around these calculations often fuels public distrust and concerns about price gouging.
Pricing Models and Profit Margins
Pharmaceutical companies utilize various pricing models, and there’s little standardization across the industry. Some companies may opt for a value-based pricing model, arguing that the significant clinical benefit justifies the high cost. Others may use a cost-plus pricing model, adding a markup to the estimated R&D and manufacturing costs. A third approach might involve price anchoring, setting a high initial price and then potentially offering discounts or rebates later.
The profit margins associated with these medicines are generally substantial, although precise figures are rarely publicly disclosed. However, the sheer price point of these treatments, coupled with the limited number of patients requiring them, points to significant profit potential for the companies involved. For example, a hypothetical drug costing $3 million per dose, even with a relatively low market share, could generate billions in revenue if only a small percentage of eligible patients receive treatment.
Influence of R&D Costs, Market Demand, and Patent Protection
The high R&D costs associated with developing genomic medicines are frequently cited as a key driver of their high prices. The complexity of genomic research, the need for extensive clinical trials, and the specialized manufacturing processes all contribute to substantial investment requirements. However, the relationship between R&D investment and final pricing is not always straightforward. Market demand also significantly influences pricing decisions.
If a genomic medicine targets a rare disease with a small patient population, the high cost per dose might be justified by the limited market size. Conversely, a drug treating a common disease with a large market might be priced lower due to economies of scale. Finally, patent protection plays a critical role. Exclusive patent rights allow pharmaceutical companies to maintain high prices for a period, maximizing profits before generic competition enters the market.
This monopoly power is a major factor in the pricing landscape of genomic medicines. The length of patent protection and the strength of the patent itself directly impact pricing decisions. Companies often strategically file multiple patents to extend their market exclusivity and maintain high prices for longer periods.
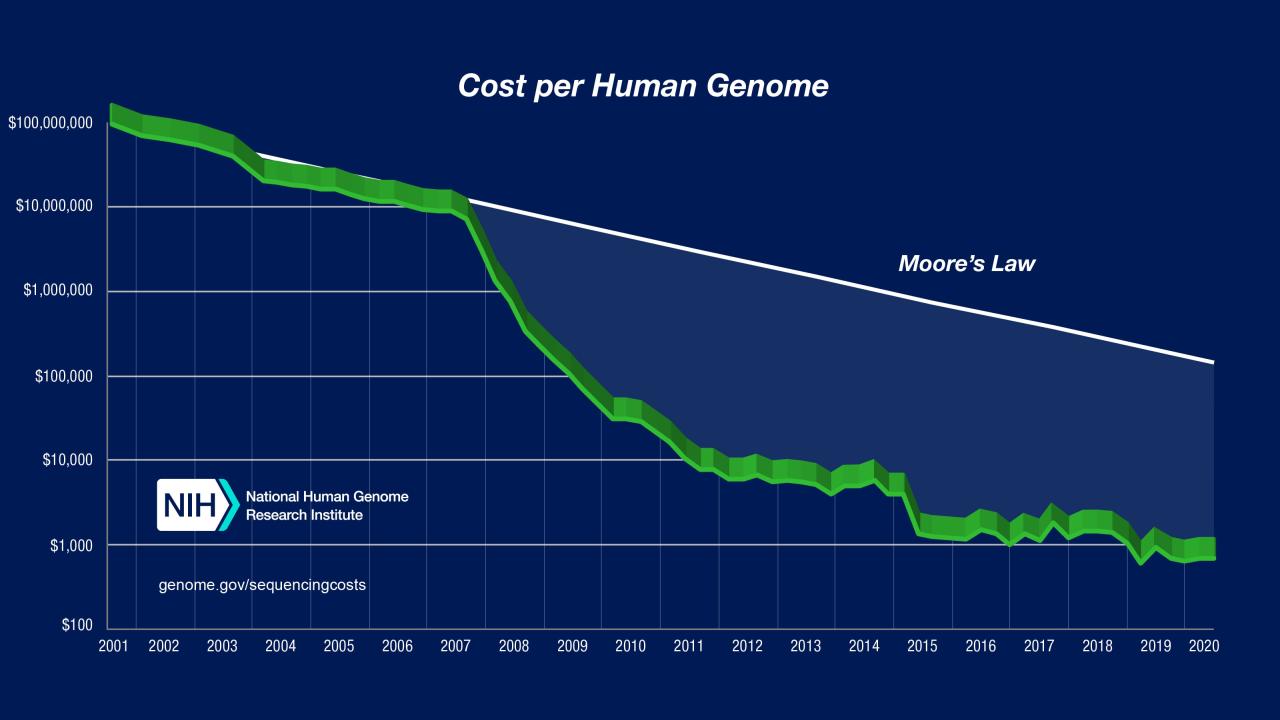
Technological Advancements and Cost Reduction
The prohibitive cost of genomic medicines, often exceeding $3 million per dose, necessitates a radical shift in production methodologies. Technological advancements offer a promising pathway towards making these life-saving treatments more accessible and affordable. By streamlining processes, improving efficiency, and accelerating drug discovery, technological innovation can significantly reduce the overall cost of genomic medicine production.Technological advancements are poised to revolutionize the cost structure of genomic medicine production.
Automation and process optimization, particularly in areas like DNA sequencing, gene synthesis, and drug formulation, can drastically reduce labor costs and increase throughput. The integration of artificial intelligence and machine learning holds the key to accelerating drug discovery and development, minimizing the time and resources required to bring new therapies to market.
Automation and Process Optimization in Genomic Medicine Production
Automation offers substantial cost savings across various stages of genomic medicine production. High-throughput screening platforms, for example, can significantly reduce the time and resources needed to identify potential drug candidates. Robotic systems can automate tasks such as sample preparation, DNA sequencing, and drug formulation, leading to increased efficiency and reduced labor costs. Process optimization techniques, such as continuous manufacturing and flow chemistry, can improve yield, reduce waste, and enhance overall efficiency.
For instance, imagine a fully automated facility where robots handle samples, run analyses, and synthesize drugs with minimal human intervention – a scenario that would significantly reduce the operational costs compared to a traditional, labor-intensive approach. This leads to a potential cost reduction of 20-30% in manufacturing alone.
Artificial Intelligence and Machine Learning in Drug Discovery and Development
AI and machine learning are transforming drug discovery and development, accelerating the identification and validation of drug targets, and optimizing drug design. AI algorithms can analyze vast datasets of genomic information to identify potential drug targets with greater accuracy and speed than traditional methods. Machine learning models can predict the efficacy and safety of drug candidates, reducing the need for costly and time-consuming clinical trials.
Consider the example of Atomwise, a company using AI to discover new drug candidates. Their AI platform has significantly reduced the time and cost associated with identifying potential treatments for various diseases, demonstrating the potential for AI to drastically reduce the overall cost of drug development. The reduction in the time to market can represent savings of millions of dollars and years of research.
Illustrative Representation of Cost Reduction
Imagine a bar graph. The first bar represents the current cost of producing a genomic medicine, reaching a height representing $3 million. The second bar, representing the cost after implementation of automation and process optimization, is shorter, perhaps reaching a height of $2.1 million, reflecting a 30% reduction. The third bar, illustrating the cost after the integration of AI and machine learning, is even shorter, perhaps reaching $1.5 million, representing an additional cost reduction.
This visual representation effectively demonstrates the potential for significant cost reduction through technological advancements.
The high cost of genomic medicines presents a significant challenge, but it’s not insurmountable. By understanding the complex interplay of research, development, regulation, and market forces, we can begin to implement effective solutions. Innovative financing models, technological advancements, and strong patient advocacy are all vital components in ensuring equitable access to these life-changing therapies. The future of genomic medicine hinges on our collective commitment to making these treatments affordable and accessible for everyone, regardless of their socioeconomic status.
The journey towards affordability requires collaboration, innovation, and a shared dedication to a healthier future.

