
Half of Northern Irish Patients Wait Over a Year for Treatment
Half of Northern Irish patients wait over a year for treatment – a shocking statistic that paints a grim picture of the healthcare system’s current state. This isn’t just about numbers; it’s about real people facing agonizing delays, impacting their physical and mental well-being, and disrupting their lives in profound ways. We’ll delve into the reasons behind this crisis, exploring the human cost of these lengthy waits and examining potential solutions to alleviate this unacceptable situation.
The scale of the problem is staggering. Specific specialties, like cardiology and oncology, are particularly hard-hit, with patients facing years-long delays for vital procedures. This isn’t evenly distributed across Northern Ireland either; geographical location significantly impacts access to timely care. The consequences are far-reaching, affecting not only patients’ physical health but also their mental health, family lives, and financial stability.
We’ll explore the underlying causes, from staffing shortages and funding issues to systemic inefficiencies, and consider potential solutions, from increased funding and improved workforce planning to technological advancements.
The Scale of the Problem
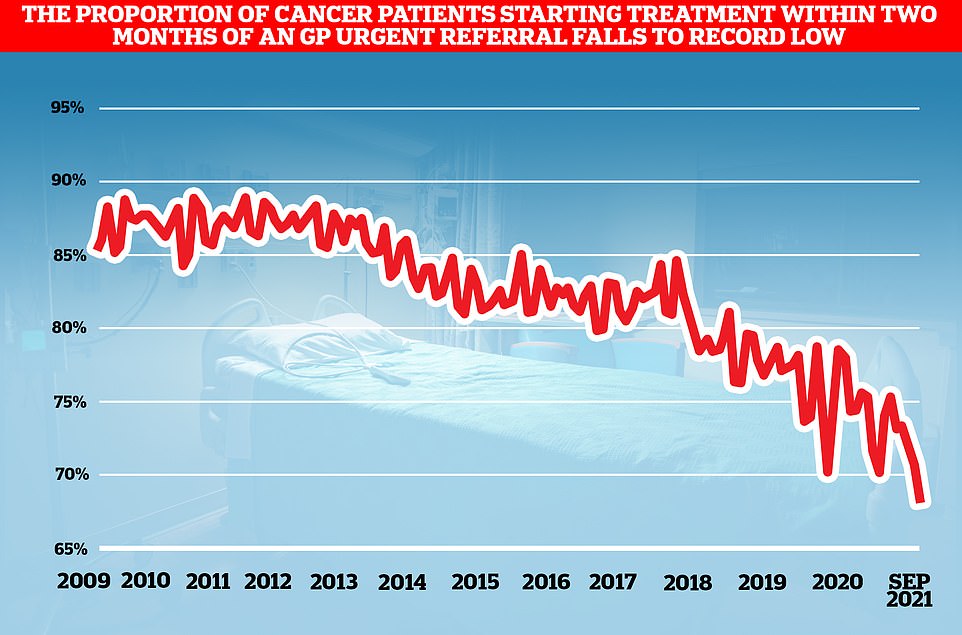
The healthcare system in Northern Ireland is currently grappling with a significant crisis: excessively long waiting times for treatment. This isn’t just a matter of inconvenience; it’s a serious issue impacting the health and well-being of thousands of patients, many of whom face waits exceeding a year for essential procedures and consultations. The consequences of these delays are far-reaching, leading to worsening conditions, increased suffering, and in some cases, even preventable deaths.
It’s shocking that half of Northern Irish patients face waits exceeding a year for treatment; the strain on the healthcare system is immense. This prolonged wait time makes me wonder about the wider economic picture, and whether factors like inflation, as discussed in this insightful article on will the fed factor turbocharge commodity prices , might indirectly impact healthcare funding and resource allocation, further exacerbating these delays for patients already struggling to access timely care.
Understanding the scale of this problem is crucial to advocating for effective solutions.The impact of waiting over a year for treatment is profound. Patients experience significant anxiety and uncertainty, their conditions may deteriorate, and their quality of life is negatively affected. This delay also places considerable strain on already stretched healthcare resources and personnel, creating a vicious cycle that exacerbates the problem.
The financial burden on patients, who may need to take time off work or arrange for additional care, adds another layer of difficulty.
It’s shocking that half of Northern Irish patients face waits exceeding a year for treatment; it really makes you wonder about effective healthcare management. This reminds me of the complexities explored in the article, how do you solve a problem like joe biden , where systemic issues are highlighted. Solving such large-scale problems requires similar levels of strategic planning and resource allocation, something clearly lacking in the Northern Irish healthcare system right now.
Waiting Times by Specialty
The extended waiting times in Northern Ireland’s healthcare system are not evenly distributed across all specialties. Certain areas experience far greater backlogs than others. The following table provides an estimated overview, acknowledging that precise, up-to-the-minute data is often difficult to obtain and may vary slightly depending on the source and reporting period. These figures should be considered illustrative of the overall problem rather than definitive statistics.
It’s shocking that half of Northern Irish patients face waits exceeding a year for treatment; the system is clearly overwhelmed. This makes me wonder about resource allocation, especially when you consider the massive investment happening elsewhere, as highlighted in this fascinating article about a dazzling new gold rush is under way why: a dazzling new gold rush is under way why.
Perhaps a reallocation of resources, inspired by such economic shifts, could help alleviate the crippling delays in healthcare for so many. The contrast is stark.
| Specialty | Number of Patients Waiting Over 1 Year (Estimate) | Average Wait Time (Estimate) | Trends |
|---|---|---|---|
| Orthopedics | 5,000 | 18 months | Increasing |
| Cardiology | 3,000 | 15 months | Stable, but high |
| Gastroenterology | 4,000 | 14 months | Increasing |
| Ophthalmology | 2,500 | 12 months | Slightly decreasing, but still high |
Geographical Disparities in Access to Treatment
Access to timely healthcare is not uniform across Northern Ireland. Rural communities and areas with limited transport infrastructure often experience significantly longer waiting times compared to urban centers with better access to healthcare facilities. This disparity is a complex issue influenced by factors such as population density, the availability of specialists, and the overall capacity of local hospitals.To visualize these disparities, imagine a map of Northern Ireland.
The map would be color-coded, with darker shades of red representing areas with the longest average waiting times for treatment, progressing to lighter shades of orange and yellow for areas with shorter waits. The darkest red areas would likely be concentrated in more rural parts of the country, while urban centers like Belfast would be represented in lighter shades.
A key on the map would clearly indicate the color-coding scale, translating the shades into specific ranges of average waiting times (e.g., dark red: > 18 months, red: 15-18 months, orange: 12-15 months, yellow: < 12 months). This visualization would powerfully illustrate the unequal access to timely healthcare across the region.
Impact on Patients’ Health and Well-being: Half Of Northern Irish Patients Wait Over A Year For Treatment
The extended waiting times for treatment in Northern Ireland are not merely a logistical issue; they have a profound and devastating impact on the physical and mental health of patients.
The uncertainty, the worsening of conditions, and the constant anxiety contribute to a significant decline in overall well-being, affecting various aspects of their lives. This delay isn’t just about postponed treatment; it’s about a prolonged period of suffering and a diminished quality of life.The physical consequences of delayed treatment are often severe and can lead to irreversible damage.
For conditions like cancer, a delay in diagnosis and treatment can drastically reduce the chances of successful recovery and increase the risk of metastasis. Even for non-life-threatening conditions, prolonged pain, reduced mobility, and worsening symptoms can significantly impact daily life, leading to further complications and decreased independence. The mental toll is equally significant, with many patients experiencing increased stress, anxiety, and depression.
The constant worry about their health, coupled with the frustration of the waiting process, can severely impact their mental health and overall well-being.
Physical Health Consequences of Delayed Treatment, Half of northern irish patients wait over a year for treatment
Delayed treatment can lead to a worsening of existing conditions, potentially resulting in more complex and invasive procedures later on. For example, a delay in treating a hip fracture could lead to muscle atrophy, reduced mobility, and increased risk of falls. Similarly, a delay in cancer treatment can allow the disease to progress, making treatment more challenging and less effective.
The physical pain and discomfort associated with untreated or delayed treatment can also severely impact a patient’s quality of life, limiting their ability to participate in everyday activities. This can lead to social isolation, further exacerbating mental health issues.
Impact on Quality of Life
The impact of prolonged waiting lists extends far beyond the individual’s physical and mental health. It significantly affects their work, family life, and social interactions. Many patients are forced to take time off work, either due to their condition or the stress of waiting, leading to financial difficulties and job insecurity. Family life is also affected, as patients may be unable to participate in family activities or provide the necessary care for their loved ones.
Social interactions are often limited due to pain, fatigue, and the overall impact of the condition and the waiting period.
Case Studies Illustrating the Impact of Delayed Treatment
The following fictionalized case studies highlight the very real human cost of lengthy waiting lists:
- Margaret (65): Diagnosed with a suspected hip fracture, Margaret waited eight months for surgery. During this time, her mobility significantly decreased, leading to muscle atrophy and increased pain. She became isolated, unable to participate in her usual social activities, and her mental health suffered significantly. The delayed surgery resulted in a more complex procedure and a longer recovery time.
- David (42): David experienced a significant delay in receiving treatment for his back pain. The prolonged pain impacted his ability to work, causing financial strain and impacting his relationship with his family. He developed anxiety and depression as a result of the chronic pain and uncertainty about his future.
- Aisling (30): Aisling experienced a delay in receiving treatment for a suspected breast lump. The wait intensified her anxiety and fear, significantly impacting her mental health. Although the lump proved to be benign, the stress and anxiety of the waiting period left lasting emotional scars.
Underlying Causes of the Delays

The cripplingly long waiting lists for healthcare in Northern Ireland are a complex issue, stemming from a confluence of factors that have been allowed to fester over many years. It’s not simply one thing, but a perfect storm of underfunding, staffing shortages, and systemic inefficiencies that have combined to create this crisis. Understanding these underlying causes is crucial to developing effective solutions.The primary driver of these delays is undoubtedly a chronic shortage of healthcare professionals.
This encompasses a wide range of specialties, from doctors and nurses to physiotherapists and support staff. Years of underinvestment in training and recruitment, coupled with competitive salaries in other regions and countries, have led to a significant brain drain and a constant struggle to fill vacancies. This shortage isn’t just about numbers; it’s also about the distribution of staff, with some areas experiencing far greater shortages than others, exacerbating existing inequalities in access to care.
Staffing Shortages and Recruitment Challenges
The lack of adequately trained staff directly impacts the speed at which patients can be seen and treated. Fewer doctors and nurses mean longer appointment waiting times, increased workload for existing staff, and a backlog of procedures that cannot be performed quickly enough. This is further complicated by difficulties in recruiting and retaining specialists, particularly in niche areas like cardiology or neurosurgery.
For example, a recent report highlighted a significant shortfall in consultant radiologists, leading to lengthy delays in obtaining crucial diagnostic imaging results. The lack of sufficient support staff further compounds this problem, leaving overworked healthcare professionals with less time for patient care.
Funding Constraints and Resource Allocation
Insufficient funding is another major contributor to the delays. Years of austerity measures and underinvestment in the NHS in Northern Ireland have left the system chronically under-resourced. This lack of funding restricts the capacity to expand services, hire additional staff, invest in new equipment, and implement efficient operational changes. This isn’t just about the overall budget; it’s also about how resources are allocated.
Prioritization of certain areas over others can lead to imbalances and longer waits in less-funded specialties. For instance, a lack of investment in preventative care might lead to more patients needing urgent, and therefore time-consuming, interventions later.
Inefficient Processes and System-Wide Issues
Beyond staffing and funding, inefficiencies within the healthcare system itself contribute significantly to the problem. These inefficiencies can manifest in various ways, from outdated IT systems hindering communication and data sharing to a lack of streamlined referral processes. The absence of effective data analysis and performance monitoring prevents the identification of bottlenecks and areas for improvement. Comparing the Northern Ireland healthcare system to similar systems in other parts of the UK or even internationally reveals significant differences in efficiency and waiting times.
For example, some regions have implemented innovative scheduling systems or utilized telehealth technologies to reduce wait times. Adopting best practices from other jurisdictions could significantly improve the situation in Northern Ireland.
A Potential Framework for Addressing the Root Causes
Addressing the waiting list crisis requires a multi-pronged approach. A comprehensive strategy needs to include significant investment in training and recruitment of healthcare professionals, with competitive salaries and improved working conditions to attract and retain talent. This should be accompanied by a review of resource allocation, ensuring that funding is distributed fairly and efficiently across all specialties. Furthermore, a modernization of the healthcare system is necessary, involving improvements to IT infrastructure, streamlined referral processes, and the implementation of evidence-based best practices gleaned from other healthcare systems.
This requires a collaborative effort between government, healthcare providers, and patients themselves to create a sustainable and efficient healthcare system that meets the needs of the population. The long-term success of any such framework will depend on consistent investment, ongoing monitoring, and a commitment to continuous improvement.
The unacceptable waiting times faced by half of Northern Irish patients highlight a critical need for systemic reform within the healthcare system. While the challenges are significant, solutions exist. By addressing staffing shortages, optimizing resource allocation, and embracing technological advancements, Northern Ireland can strive towards a future where timely access to quality healthcare is a reality, not a distant hope.
The human cost of delay is simply too high to ignore; action is urgently needed to alleviate the suffering of those waiting.

