How AI Could Transform Medical Research and Treatment
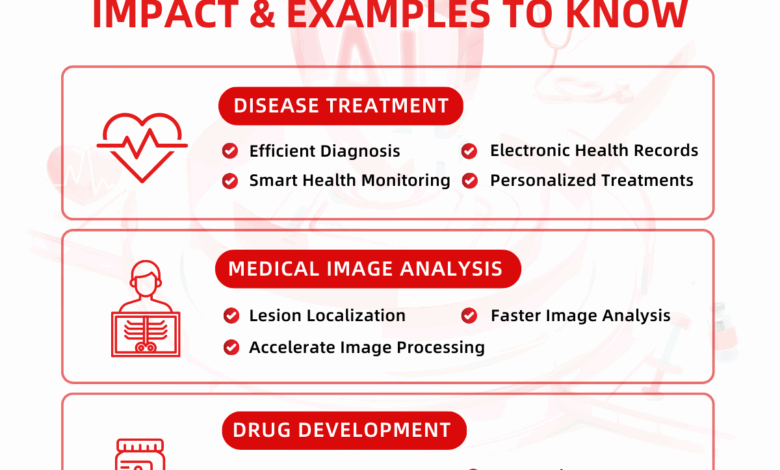
How AI could transform medical research and treatment is a question that’s rapidly moving from science fiction to reality. We’re on the cusp of a medical revolution, where artificial intelligence isn’t just a tool, but a potential game-changer, impacting everything from drug discovery to personalized medicine. This post delves into the exciting possibilities – and the challenges – that lie ahead as AI reshapes healthcare as we know it.
Imagine a future where diseases are diagnosed earlier and more accurately, where treatments are tailored to individual patients, and where complex surgeries are performed with unprecedented precision. That future is being built, brick by brick, with the help of AI. From analyzing medical images to designing more effective drugs, AI is already making significant contributions. This exploration will cover AI’s role in drug development, medical imaging, personalized medicine, robotic surgery, public health, and clinical trial management, painting a picture of both the potential benefits and the ethical considerations we need to address.
Personalized Medicine and Treatment Plans

The era of one-size-fits-all medicine is rapidly fading. AI is poised to revolutionize healthcare by enabling the creation of truly personalized treatment plans, tailored to the unique genetic makeup, medical history, and lifestyle of each individual patient. This shift promises to significantly improve treatment efficacy, reduce adverse effects, and ultimately enhance patient outcomes.AI’s ability to analyze vast amounts of complex data is the key driver of this transformation.
By integrating genomic information, electronic health records, lifestyle data (diet, exercise, sleep patterns), and even wearable sensor data, AI algorithms can identify patterns and correlations that would be impossible for humans to detect manually. This detailed understanding allows for the development of highly specific and effective treatments.
AI-Driven Analysis of Patient Data for Personalized Treatment
AI algorithms can sift through a patient’s complete medical profile, identifying genetic predispositions to certain diseases, analyzing the effectiveness of past treatments, and even predicting potential risks based on lifestyle factors. For example, AI can identify specific gene mutations that contribute to a patient’s cancer and then recommend targeted therapies that are more likely to be successful. Similarly, by analyzing a patient’s lifestyle data, AI can identify potential risk factors for cardiovascular disease and recommend preventative measures, such as dietary changes or increased physical activity.
This level of personalized insight empowers both patients and healthcare providers to make informed decisions.
AI’s Role in Predicting Treatment Response and Optimizing Strategies
Predicting how a patient will respond to a particular therapy is a major challenge in medicine. AI is proving invaluable in this area. Machine learning models can be trained on large datasets of patient information and treatment outcomes to predict the likelihood of success for different therapies. This predictive capability allows doctors to select the most effective treatment from the outset, minimizing the time and resources spent on trial-and-error approaches.
Furthermore, AI can continuously monitor a patient’s response to treatment, adjusting the dosage or treatment strategy as needed to optimize outcomes and minimize side effects. This adaptive approach ensures that treatment remains effective and safe throughout the course of the disease.
Hypothetical Scenario: Personalized Cancer Treatment Plan
Let’s imagine a scenario involving a patient diagnosed with breast cancer.
AI’s potential in medicine is huge – imagine personalized treatments based on individual genetic profiles! But even this relies on incredible computational power, and the advancements needed are mind-boggling; consider that, as explained in this fascinating article on node names do not reflect actual transistor sizes , the technology behind the scenes is far more complex than we often realize.
Ultimately, this underlying hardware pushes the boundaries of what AI can achieve in accelerating medical breakthroughs, paving the way for faster diagnoses and more effective cures.
- Data Collection: The patient’s complete medical history, including genomic data (obtained through a biopsy), imaging scans, and lifestyle information, is collected and input into an AI system.
- Genomic Analysis: AI analyzes the patient’s genomic data, identifying specific mutations that drive the cancer’s growth. It identifies the presence of HER2 receptors, indicating a specific type of breast cancer.
- Treatment Recommendation: Based on the genomic analysis and other factors, the AI system suggests a personalized treatment plan. In this case, it recommends targeted therapy with a drug specifically designed to inhibit HER2 receptors, alongside a carefully tailored chemotherapy regimen.
- Treatment Monitoring and Adjustment: Throughout the treatment, the AI system continuously monitors the patient’s response, tracking tumor size, side effects, and other relevant indicators. If the cancer shows resistance to the initial treatment, the AI suggests alternative therapies or adjustments to the current regimen, optimizing the approach for maximum efficacy.
- Outcome Prediction: Using historical data and the patient’s unique profile, the AI system predicts the likelihood of long-term remission and potential recurrence, enabling proactive monitoring and preventative measures.
This hypothetical scenario highlights how AI can transform cancer treatment from a generalized approach to a highly personalized strategy, significantly improving patient outcomes and quality of life. The ability to predict response, optimize treatment, and proactively manage potential risks represents a significant leap forward in cancer care.
AI-Powered Robotic Surgery and Treatment
The integration of artificial intelligence (AI) into robotic surgery is revolutionizing the medical field, promising increased precision, minimized invasiveness, and faster patient recovery. AI algorithms are enhancing the capabilities of robotic surgical systems in ways previously unimaginable, leading to significant advancements in various surgical specialties. This technology is not just about automation; it’s about augmenting the surgeon’s skills and capabilities, ultimately leading to better patient outcomes.AI is enhancing robotic surgery in several key ways.
AI’s potential in medicine is mind-blowing – imagine faster drug discovery and personalized treatments! It’s amazing how collaborative problem-solving works, like what’s happening with true crime fans are banding together online to try to solve cases , and that same spirit could revolutionize medical research. Think of AI sifting through massive datasets to identify patterns and accelerate breakthroughs – it’s a whole new era of collaborative medical advancement!
It’s no longer just a matter of remotely controlled robotic arms; AI is providing real-time assistance and analysis, improving the surgeon’s decision-making process.
Examples of AI Enhancement in Robotic Surgery
AI algorithms are being used to improve the precision of robotic surgical movements. For example, systems can analyze real-time images from the surgical field to provide haptic feedback to the surgeon, giving them a more nuanced sense of touch and allowing for finer control during delicate procedures. This is particularly useful in microsurgery, such as in neurosurgery or ophthalmology, where precision is paramount.
Furthermore, AI can help with tasks like tissue identification and real-time assessment of bleeding, providing surgeons with crucial information to make better decisions during the procedure. One example is the use of AI to identify cancerous tissue during tumor resection, enabling more complete removal and potentially improving survival rates. Another application is the use of AI-powered image analysis to guide the placement of surgical instruments, reducing the risk of damage to surrounding healthy tissue.
Potential for Autonomous and Semi-Autonomous Robotic Surgery
The long-term vision for AI in robotic surgery involves the development of autonomous or semi-autonomous systems capable of performing complex procedures with minimal human intervention. While fully autonomous surgery is still some way off, research is progressing rapidly. Current semi-autonomous systems already assist surgeons with tasks such as suturing, tissue dissection, and instrument manipulation, improving efficiency and reducing surgeon fatigue.
AI’s potential in medicine is mind-blowing – imagine faster drug discovery and personalized treatments! It’s a high-stakes game, much like the ventures of Masayoshi Son, whose life story, as detailed in this article , shows the kind of bold bets needed for major breakthroughs. Ultimately, AI could revolutionize healthcare, offering hope where previously there was none.
These systems are trained on vast datasets of surgical procedures, allowing them to learn and adapt to different situations. For example, a semi-autonomous system might be used to assist in laparoscopic cholecystectomy (gallbladder removal), autonomously performing tasks like dissecting the gallbladder from surrounding tissues under the surgeon’s supervision. This allows the surgeon to focus on more complex aspects of the procedure, improving overall efficiency and potentially reducing the length of the surgery.
Ethical Considerations and Challenges of AI in Surgical Procedures
The increasing use of AI in surgical procedures presents a number of ethical considerations and challenges that require careful attention. It’s crucial to establish clear guidelines and regulations to ensure the safe and responsible implementation of this technology.
The following points highlight potential benefits and risks:
- Benefits: Improved surgical precision and accuracy, reduced invasiveness, shorter recovery times, increased efficiency, potential for improved access to surgical care in remote areas, reduced surgeon fatigue and errors.
- Risks: Potential for algorithmic bias leading to disparities in care, dependence on technology potentially reducing surgeon skills, cybersecurity vulnerabilities, liability issues in case of malfunction, lack of transparency in AI decision-making processes, ethical concerns regarding autonomous decision-making by AI in life-or-death situations.
AI in Public Health and Disease Surveillance
The integration of artificial intelligence (AI) into public health is revolutionizing our ability to monitor, predict, and respond to disease outbreaks. AI’s capacity to process and analyze massive datasets far surpasses human capabilities, offering unprecedented opportunities for proactive and effective public health interventions. This enhanced surveillance allows for quicker responses, potentially saving lives and minimizing the impact of epidemics.AI algorithms can analyze diverse public health data, including electronic health records, social media posts, weather patterns, and geographical information systems (GIS) data, to identify patterns and anomalies indicative of emerging disease outbreaks.
This real-time monitoring allows for rapid detection of unusual clusters of illnesses, significantly reducing the time lag between initial infection and public health response.
Disease Outbreak Identification and Prediction
AI algorithms, particularly machine learning models, excel at identifying subtle patterns within complex datasets that might be missed by human analysts. For example, an AI system might detect a statistically significant increase in hospital admissions for pneumonia in a specific region, even if the individual reports don’t immediately suggest an epidemic. By cross-referencing this data with other sources, such as social media posts mentioning flu-like symptoms in the same area, the AI can generate an alert flagging a potential outbreak, enabling public health officials to investigate and implement preventative measures promptly.
This predictive capability is particularly crucial for rapidly spreading infectious diseases. Predictive models, trained on historical data of past outbreaks, can forecast the potential trajectory of a new outbreak, considering factors like population density, mobility patterns, and climate conditions.
Tracking the Spread of Infectious Diseases
Imagine a dynamic, interactive map. This map displays the geographical spread of a disease in real-time, updated continuously as new data streams in. Each dot represents a confirmed case, color-coded by severity or date of onset. The size of the dot might reflect the number of cases in a specific location. The AI system, powering this map, uses advanced algorithms to analyze data from various sources—hospital reports, laboratory results, and even anonymized mobile phone location data—to project the potential spread of the disease.
It can identify high-risk areas, predict the number of expected cases, and even simulate different intervention scenarios (e.g., implementing quarantine measures in specific regions) to determine the most effective course of action. This real-time tracking allows public health authorities to allocate resources effectively and target interventions where they are most needed. For instance, during the COVID-19 pandemic, AI-powered models helped predict hospital bed capacity needs and optimize the distribution of personal protective equipment.
Modeling Disease Spread and Predicting Population Impact
A visual representation of AI’s predictive capabilities could be a 3D model. This model displays a geographical area, perhaps a city or region, with a translucent overlay representing the predicted spread of a disease over time. The intensity of the color in the overlay increases as the predicted number of cases rises in that area. Different colors might represent different stages of the disease, such as suspected cases, confirmed cases, and recoveries.
The model might also show projections of the impact on the healthcare system, such as hospital bed occupancy and ICU capacity, illustrating the potential strain on resources. For example, an AI model could simulate the impact of a new influenza strain, factoring in vaccination rates, population demographics, and the strain’s transmissibility to predict the peak infection rate and the overall number of hospitalizations and deaths.
This would allow for better resource allocation, planning for potential shortages, and targeted public health campaigns.
AI for Clinical Trial Design and Management: How Ai Could Transform Medical Research And Treatment

The pharmaceutical industry faces significant challenges in bringing new therapies to market, including lengthy timelines, high costs, and low success rates. AI offers a powerful toolkit to address these hurdles, streamlining the clinical trial process from design to data analysis. By leveraging AI’s capabilities in data analysis, prediction, and automation, we can significantly improve efficiency and effectiveness.AI’s role in clinical trial design and management is rapidly expanding, impacting nearly every stage of the process.
From optimizing patient recruitment strategies to accelerating data analysis and interpretation, AI promises to revolutionize how we develop and test new treatments. This leads to faster development of life-saving medications and therapies.
AI Optimization of Clinical Trial Design
AI algorithms can analyze vast datasets of patient information, historical trial data, and relevant medical literature to identify optimal trial designs. This includes determining the appropriate sample size, selecting suitable patient populations, defining endpoints, and optimizing treatment regimens. For instance, AI can predict the likelihood of a trial’s success based on various factors, enabling researchers to make data-driven decisions early in the process, minimizing wasted resources on trials unlikely to succeed.
This predictive power also helps in identifying potential confounding factors and adjusting the design accordingly, leading to more robust and reliable results. Machine learning models can even suggest novel trial designs that may not have been considered using traditional methods, pushing the boundaries of clinical research.
AI-Powered Patient Recruitment
Recruiting suitable participants for clinical trials is often a significant bottleneck. AI can significantly improve recruitment efficiency by identifying potential participants from diverse sources, including electronic health records (EHRs), social media, and patient registries. AI-powered algorithms can analyze patient data to identify individuals who meet specific inclusion and exclusion criteria, greatly reducing the time and resources spent on manual screening.
Furthermore, AI can personalize recruitment messages, tailoring them to individual patients’ preferences and concerns, increasing the likelihood of participation. Targeted advertising campaigns, powered by AI, can also significantly improve recruitment outcomes. For example, an AI system could identify individuals with specific genetic predispositions to a particular disease, making targeted recruitment significantly more effective.
AI in Clinical Trial Data Analysis
Traditional methods of analyzing clinical trial data often rely on statistical methods that may overlook subtle patterns or complex interactions between variables. AI, particularly machine learning, can analyze large and complex datasets to identify patterns and insights that might be missed by human analysts. This includes identifying subgroups of patients who respond differently to treatment, discovering unexpected correlations between variables, and predicting treatment outcomes with greater accuracy.
For instance, AI can help detect adverse events that may not be immediately apparent, improving patient safety. AI-driven analysis can also uncover biomarkers that predict treatment response, enabling the development of more personalized therapies. This can lead to a better understanding of disease mechanisms and improved drug development.
Comparison of AI-Driven and Traditional Clinical Trial Management, How ai could transform medical research and treatment
The following table compares three key aspects of AI-driven and traditional clinical trial management:
| Aspect | AI-Driven Approach | Traditional Approach |
|---|---|---|
| Patient Recruitment | Faster, more targeted, higher success rates through AI-powered identification and personalized messaging. | Slower, less targeted, reliant on manual screening and broad advertising, often resulting in lower participation rates. |
| Data Analysis | Identifies subtle patterns and complex interactions, leading to more robust and reliable conclusions. Faster processing of large datasets. | Relies primarily on statistical methods, potentially missing subtle patterns and interactions; slower processing of large datasets. |
| Trial Design Optimization | Data-driven design optimization, leading to more efficient and effective trials. Predictive modeling to minimize failure rates. | Relies on expert opinion and historical data, potentially leading to suboptimal designs and increased failure rates. |
The integration of AI into medical research and treatment is poised to revolutionize healthcare, offering the potential for faster diagnoses, more effective treatments, and improved patient outcomes. While challenges remain, particularly concerning data privacy, algorithmic bias, and ethical considerations surrounding autonomous systems, the potential benefits are too significant to ignore. The journey ahead will require careful collaboration between AI developers, healthcare professionals, and policymakers to ensure responsible and equitable implementation.
The future of medicine is intelligent, and it’s unfolding before our eyes.
