Why Open Source AI Models Are Good for the World
Why open source AI models are good for the world? It’s a question that deserves a deep dive. We’re living in a time where artificial intelligence is rapidly transforming our lives, and the way these models are developed and shared has profound implications. Open-source AI isn’t just about code; it’s about democratizing access, fostering collaboration, and ultimately, building a better future.
This post explores how open source AI is leveling the playing field, accelerating innovation, and tackling some of humanity’s biggest challenges.
From healthcare advancements to tackling climate change, the potential applications are vast and the benefits are undeniable. By removing the barriers to entry associated with proprietary models, open source empowers individuals and organizations worldwide to participate in the AI revolution, leading to faster progress and more equitable outcomes. We’ll examine specific examples, explore the economic benefits, and delve into the ethical considerations that shape this rapidly evolving landscape.
Increased Accessibility and Democratization of AI
Open-source AI models are revolutionizing the field by dramatically lowering the barrier to entry for researchers, developers, and businesses of all sizes. This democratization of access to advanced AI technologies fosters wider participation and accelerates innovation across numerous sectors, leading to more equitable and impactful applications. The availability of open-source models removes significant financial and technical hurdles, empowering individuals and organizations previously excluded from AI development.Open-source AI models significantly reduce the cost and complexity associated with developing and deploying AI solutions.
Unlike proprietary models, which often require substantial licensing fees and specialized expertise, open-source alternatives provide free access to the underlying code, allowing researchers and developers to adapt, modify, and extend the models to meet their specific needs. This fosters a collaborative environment where advancements are shared freely, accelerating the pace of innovation.
Examples of Open-Source AI Projects and Their Impact
The open-source AI community has produced numerous impactful projects. For instance, in healthcare, OpenAI’s GPT models have been adapted for tasks such as medical diagnosis support and drug discovery. The open-source nature of these models allows researchers worldwide to fine-tune them for specific medical applications, potentially leading to faster diagnoses and more effective treatments. In education, projects like TensorFlow and PyTorch have enabled the creation of personalized learning platforms and intelligent tutoring systems.
These platforms leverage open-source AI models to analyze student performance, adapt learning materials, and provide customized feedback, leading to improved learning outcomes. These are just a few examples showcasing the transformative power of open-source AI in various sectors.
Cost and Accessibility Comparison: Open-Source vs. Proprietary AI Models
The following table highlights the key differences in cost and accessibility between open-source and proprietary AI models. Note that these are general comparisons and specific costs can vary greatly depending on the model, scale of deployment, and required computational resources.
| Feature | Open-Source AI Models | Proprietary AI Models |
|---|---|---|
| Training Data | Often requires sourcing and preparing your own data, potentially incurring costs. However, publicly available datasets are frequently used. | Typically includes pre-trained models with proprietary datasets, reducing data acquisition costs but limiting customization. |
| Computational Resources | Requires access to computational resources (GPUs, TPUs, etc.), which can be costly depending on the model size and training duration. Cloud computing offers scalable options. | Often requires access to cloud services offered by the proprietary model provider, leading to recurring costs tied to usage. |
| Licensing Fees | Generally free, but may involve costs associated with commercial deployment or specific support services. | Significant upfront and/or recurring licensing fees are common, often dependent on usage volume and specific features. |
| Accessibility | High accessibility due to freely available code and documentation. However, expertise in AI and programming is often required. | Accessibility is limited by cost and the need for specific agreements or partnerships with the proprietary model provider. |
Fostering Innovation and Collaboration
Open-source AI models aren’t just about sharing code; they’re about fostering a vibrant ecosystem of collaboration that dramatically accelerates the pace of innovation. The collaborative spirit inherent in open-source development allows for a rapid exchange of ideas, expertise, and resources, leading to breakthroughs that would be significantly slower, if possible at all, in a proprietary setting. This shared effort translates to faster iteration cycles, quicker bug fixes, and a more robust and reliable final product.The collaborative nature of open-source projects allows for a diversity of perspectives and skill sets to contribute to a single project.
This distributed intelligence often results in more creative solutions and a more thorough vetting process, leading to higher-quality AI models. Unlike proprietary development, where progress is often confined within the walls of a single company, open-source AI thrives on the collective brainpower of a global community. This means faster problem-solving, quicker adaptation to new challenges, and a more resilient AI ecosystem overall.
Examples of Collaborative Open-Source AI Projects
The success of open-source AI is best illustrated through examining real-world examples. Projects like TensorFlow and PyTorch, foundational deep learning libraries, exemplify the power of collaborative development. These projects have benefited from contributions from thousands of developers worldwide, representing a vast array of backgrounds and expertise. The resulting libraries are not only powerful and versatile but also incredibly well-documented and supported, thanks to the collective effort.
Open source AI models democratize access to powerful technology, fostering innovation and collaboration globally. This transparency is crucial, especially considering events like the recent controversy where Mohave County delayed certifying Arizona election results in protest, as reported by this news article. The openness of AI development mirrors the need for transparent and accountable processes in governance, ultimately benefiting everyone.
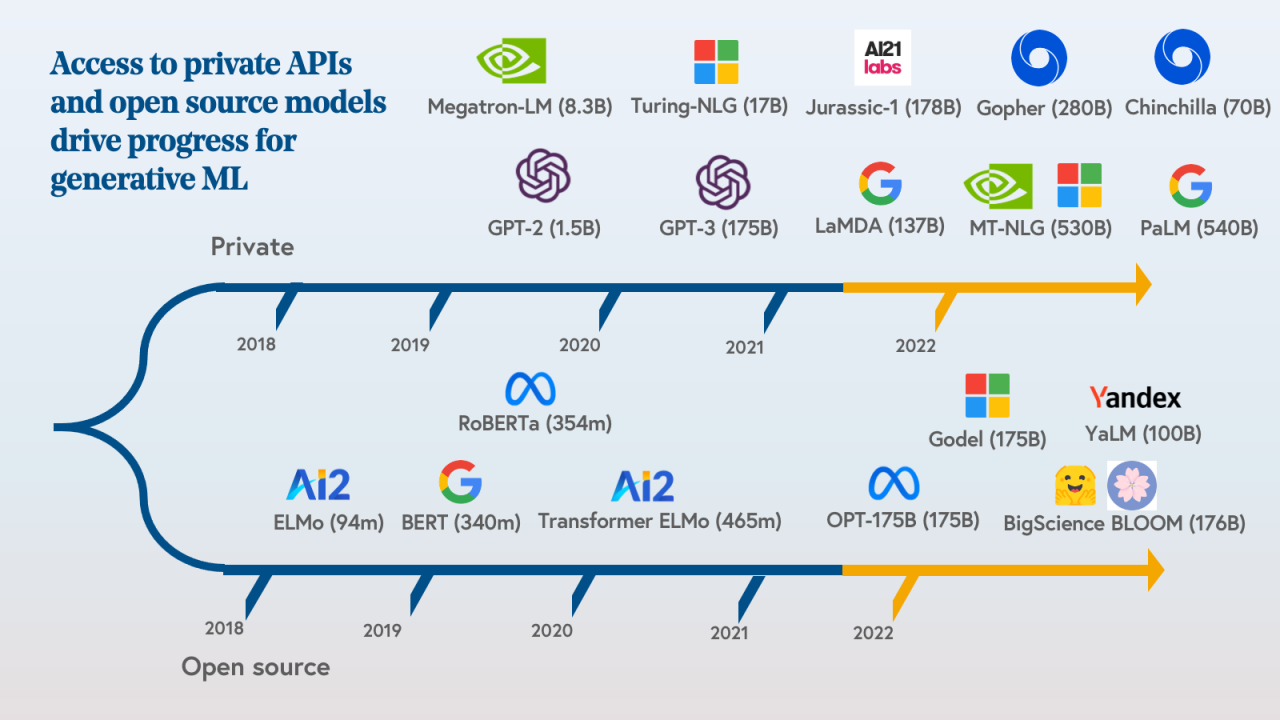
Another example is OpenAI’s work on models like GPT-3, although initially proprietary, their subsequent open-source efforts (like releasing smaller, more accessible versions) have significantly contributed to the advancement of large language models. The open-sourcing of these models allows researchers and developers to build upon existing work, leading to a more rapid evolution of the technology.
Comparison of Innovation Pace: Open-Source vs. Proprietary AI
Comparing the innovation pace between open-source and proprietary AI development reveals a stark contrast. While proprietary companies often prioritize protecting their intellectual property, leading to slower dissemination of knowledge and technology, open-source projects encourage rapid sharing and adaptation. For example, the development of new algorithms and techniques in areas like computer vision and natural language processing often sees faster adoption and refinement within the open-source community.
Open source AI models democratize access to powerful technology, leveling the playing field for researchers and developers globally. This reminds me of a recent political analysis I read, gingrich gop got nearly 6 million more votes but lost many races whats going on , highlighting how raw numbers don’t always tell the whole story. Similarly, open-source AI ensures transparency and fosters collaboration, ultimately leading to faster innovation and more beneficial applications for everyone.
A specific milestone illustrating this is the rapid advancement of generative adversarial networks (GANs). Open-source implementations and variations allowed for a quicker exploration of different architectures and applications, leading to breakthroughs that were then adopted by proprietary companies. While proprietary AI development may occasionally produce significant breakthroughs, the overall rate of innovation and the speed of technology adoption tend to be significantly faster in the open-source realm.
This is largely due to the collaborative nature of open-source projects, where progress is transparent, accessible, and built upon the work of many.
Enhanced Transparency and Trust
Open-source AI models offer a crucial advantage over proprietary systems: transparency. This transparency fosters trust by allowing independent researchers, developers, and even the general public to scrutinize the algorithms and data used. This level of access is invaluable in understanding how these models work, identifying potential biases, and ensuring responsible development. Unlike closed-source systems where the inner workings remain opaque, open-source models promote a more accountable and trustworthy AI ecosystem.The ability to examine the code and data behind an open-source AI model is a powerful tool for identifying and mitigating bias.
Bias can creep into AI systems through various sources, including skewed training data or inherent biases in the algorithms themselves. Openness allows the community to detect these biases and propose solutions, leading to fairer and more equitable outcomes. This collaborative approach to bias detection and correction is significantly more robust than relying on the internal checks and balances of a single company.
For example, the open-source community could identify a dataset over-representing a particular demographic and propose alternative, more representative data sources, leading to a less biased model.
Bias Detection and Mitigation Mechanisms in Open-Source AI
The open nature of these projects facilitates community review and improvement. Researchers and developers can contribute to identifying and correcting biases, improving model accuracy and fairness. This collaborative approach harnesses the collective intelligence of a diverse group, leading to a more robust and reliable outcome than relying on a single entity. Imagine a scenario where a bias is detected in an open-source image recognition model—a bias favoring certain ethnicities in facial recognition.
The community can then work together to identify the root cause, perhaps a skewed training dataset, and contribute code or data to correct the bias. This collaborative process is a core strength of open-source AI, ensuring ongoing refinement and improvement.
Strategies for Ensuring Transparency and Mitigating Bias
It’s crucial to implement proactive strategies to ensure transparency and mitigate bias in open-source AI projects. These strategies should be embedded throughout the development lifecycle, from data collection to model deployment.
- Comprehensive Documentation: Clearly documenting the data sources, preprocessing steps, model architecture, and training process is essential. This allows others to understand the model’s strengths and limitations and identify potential biases.
- Data Auditing and Bias Detection Tools: Utilizing tools and techniques to automatically detect and quantify bias in datasets is crucial. These tools can help identify over-representation or under-representation of specific groups and guide data augmentation or selection strategies.
- Community Review and Feedback Mechanisms: Establishing clear channels for community feedback and contribution is critical. This could involve forums, issue trackers, or dedicated review processes where users can report potential biases or suggest improvements.
- Version Control and Traceability: Using robust version control systems allows for tracking changes made to the model and data over time. This transparency helps to understand the evolution of the model and identify the source of any introduced biases.
- Regular Audits and Independent Verification: Independent audits and verification of the model’s performance and fairness should be conducted regularly to ensure ongoing adherence to ethical guidelines and best practices.
Economic Benefits and Opportunities
Open-source AI offers a compelling economic proposition, reshaping the landscape for businesses of all sizes. By reducing barriers to entry and fostering innovation, it unlocks significant opportunities for growth and competitive advantage, ultimately contributing to a more dynamic and inclusive economy. This contrasts sharply with the high costs and limited accessibility often associated with proprietary AI solutions.The core economic benefits stem from significantly reduced development costs and increased access to a diverse talent pool.
Developing AI models from scratch is incredibly expensive, requiring substantial investment in research, data acquisition, and specialized expertise. Open-source models provide a readily available foundation, allowing businesses to focus resources on customization and integration, rather than reinventing the wheel. Furthermore, the open nature of these models fosters a collaborative environment, enabling a wider range of developers and researchers to contribute to improvements and advancements, creating a larger, more diverse talent pool.
Reduced Development Costs and Access to Wider Talent Pool, Why open source ai models are good for the world
Open-source AI dramatically lowers the barrier to entry for businesses seeking to leverage AI capabilities. Instead of investing millions in developing proprietary models, companies can utilize pre-trained models, adapting them to their specific needs with comparatively smaller investments in time and resources. This translates directly to reduced operational costs and faster time-to-market for AI-powered products and services. Simultaneously, the collaborative nature of open-source projects attracts a wider pool of talent.
Open-source AI models democratize access to powerful technology, leveling the playing field for researchers and developers worldwide. This is crucial because even small-scale online activities can have tax implications, as highlighted by the recent IRS warning irs issues another tax warning to americans who made more than 600 online. The transparency of open-source AI allows for better understanding and responsible development, ultimately benefiting everyone, regardless of their income or tax bracket.
Developers and researchers from around the world contribute to these projects, leading to faster innovation cycles and the development of more robust and versatile models. This accessibility also allows smaller companies and startups, who might otherwise lack the resources to compete, to participate in the AI revolution.
Examples of Successful Businesses Leveraging Open-Source AI
Several businesses have successfully leveraged open-source AI to gain a competitive advantage. For example, many startups in the healthcare sector utilize open-source models for image analysis and disease detection, significantly reducing the cost and time required for developing diagnostic tools. Their strategy involves fine-tuning existing open-source models with their own specialized datasets, allowing them to rapidly develop and deploy effective solutions.
This approach enables them to compete with larger, more established players, resulting in quicker deployment and market penetration. Similarly, numerous companies in the financial services industry employ open-source AI for fraud detection and risk assessment, adapting existing models to their specific data and regulatory requirements. The cost savings and increased efficiency resulting from this approach allow these companies to offer more competitive services and enhance their operational efficiency.
Long-Term Economic Impacts of Open-Source vs. Proprietary AI Ecosystems
The long-term economic implications of open-source and proprietary AI ecosystems differ significantly. A proprietary ecosystem, characterized by high barriers to entry and limited access, risks creating a concentrated market dominated by a few powerful players. This can stifle innovation and limit the widespread adoption of AI technologies. In contrast, an open-source ecosystem fosters a more distributed and inclusive approach, encouraging widespread participation and collaboration.
This leads to faster innovation, broader adoption, and ultimately, greater economic benefits for society as a whole. While proprietary models might offer short-term advantages in terms of control and intellectual property, the long-term economic potential of the open-source approach, with its emphasis on collaboration and accessibility, is arguably greater. The open nature allows for faster iteration and improvement, leading to more robust and efficient AI solutions that benefit a wider range of users and industries.
This fosters a more dynamic and competitive market, ultimately driving economic growth and creating new opportunities.
Addressing Global Challenges: Why Open Source Ai Models Are Good For The World
Open-source AI offers a powerful toolset for tackling some of humanity’s most pressing global challenges. By making AI accessible to a wider range of researchers, developers, and organizations, it fosters collaboration and innovation, leading to more effective and efficient solutions than would be possible with proprietary models. This democratization of AI is crucial for addressing issues that transcend national borders and require global cooperation.Open-source AI models are already contributing to significant advancements in various fields, accelerating progress toward a more sustainable and equitable future.
The collaborative nature of open-source development allows for rapid iteration and improvement, ensuring solutions are constantly refined and adapted to evolving needs.
Climate Change Mitigation
Open-source AI can significantly aid in climate change mitigation efforts. For example, open-source machine learning models are being used to analyze satellite imagery to monitor deforestation rates and predict future trends, enabling proactive conservation measures. Other applications include optimizing energy grids for greater efficiency, improving weather forecasting accuracy for disaster preparedness, and developing more efficient renewable energy sources through simulations and predictive modeling.
The open nature of these models allows researchers globally to contribute improvements and adaptations specific to their local contexts, maximizing impact.
Disease Prevention and Healthcare Access
Open-source AI is revolutionizing healthcare, particularly in underserved communities. AI-powered diagnostic tools, trained on open datasets of medical images and patient records, can assist in early detection of diseases like malaria, tuberculosis, and various cancers. These tools can be deployed in resource-limited settings, where access to specialized medical professionals is often scarce. Furthermore, open-source platforms are facilitating the development of drug discovery and vaccine research, accelerating the pace of innovation and making vital treatments more accessible.
Poverty Reduction
Open-source AI can contribute to poverty reduction through various applications. For instance, AI-powered agricultural tools can optimize crop yields, improving food security in developing countries. Open-source models can also analyze socioeconomic data to identify vulnerable populations and allocate resources more effectively, targeting aid and development programs with greater precision. Furthermore, AI-powered educational tools can provide personalized learning experiences, improving access to quality education regardless of geographical location or socioeconomic status.
The accessibility of open-source AI makes these solutions scalable and adaptable to diverse contexts, maximizing their impact on poverty reduction efforts.
Promoting Sustainable Development and Bridging the Digital Divide
Open-source AI plays a crucial role in promoting sustainable development by providing accessible tools for monitoring environmental conditions, optimizing resource management, and developing sustainable technologies. By removing the financial barriers associated with proprietary AI, it empowers organizations and individuals in developing countries to participate actively in the global effort towards sustainable development goals. Furthermore, open-source AI contributes significantly to bridging the digital divide.
The availability of open-source tools and resources allows for the development of affordable and accessible AI solutions tailored to the specific needs of underserved communities, ensuring that the benefits of AI are not confined to a privileged few.
Improving Access to Healthcare in Underserved Communities
Imagine a visual representation: A stylized map of the world, highlighting regions with limited healthcare access in darker shades. Superimposed on this map are vibrant nodes of light, representing the deployment of open-source AI-powered diagnostic tools in clinics and hospitals within these underserved areas. Lines connecting these nodes depict the collaborative network of researchers and healthcare providers sharing data and improving the algorithms.
Each node shows a small icon representing a specific AI application, such as a microscope for disease detection, a heart monitor for remote patient monitoring, or a virtual assistant providing healthcare information in local languages. This visualization effectively illustrates how open-source AI expands healthcare access to remote and resource-constrained regions, bridging the healthcare gap and improving health outcomes for millions.
Improved Education and Skill Development
Open-source AI models are revolutionizing education, offering unparalleled access to cutting-edge AI technologies and fostering a more inclusive and collaborative learning environment. Their availability democratizes access to resources previously limited to well-funded institutions, empowering students and professionals worldwide to learn and contribute to the field. This accessibility fosters a more diverse and inclusive AI community, driving innovation and solving real-world problems.The availability of open-source AI models provides invaluable educational resources.
Students can directly interact with the models, experimenting with different parameters and observing their behavior. This hands-on approach enhances understanding far beyond theoretical lectures. Professionals can utilize these models to upskill or reskill in the rapidly evolving field of AI, keeping their knowledge current and relevant to industry demands. Furthermore, open-source models provide a platform for collaborative learning and knowledge sharing, allowing students and professionals to learn from each other’s experiences and contributions.
Educational Initiatives Leveraging Open-Source AI
Several educational initiatives are effectively utilizing open-source AI models. For instance, many universities incorporate open-source frameworks like TensorFlow and PyTorch into their AI curricula, providing students with practical experience in building and deploying AI systems. These frameworks offer extensive documentation, tutorials, and online communities, supporting self-directed learning and collaborative projects. Online platforms like fast.ai provide structured courses using open-source tools, making advanced AI concepts accessible to a wider audience.
Research institutions also leverage open-source models for collaborative research projects, fostering the development of new AI algorithms and applications. The open nature of these models encourages transparency and reproducibility, enhancing the rigor and reliability of research findings.
Benefits of Open-Source AI Across Different Education Levels
| Education Level | Accessibility of Resources | Practical Application | Community Support |
|---|---|---|---|
| Introductory | Abundant free tutorials, documentation, and pre-trained models simplify learning fundamental concepts. | Simple projects using pre-trained models allow for immediate experimentation and visualization of AI principles. | Large and active online communities offer readily available assistance and guidance for beginners. |
| Intermediate | Access to more complex models and datasets allows for deeper exploration of specific AI techniques. | Students can build and modify existing models, gaining practical experience in model training and optimization. | More specialized communities offer support for tackling advanced challenges and troubleshooting complex issues. |
| Advanced | Open-source research papers and codebases provide insights into state-of-the-art AI algorithms. | Students can contribute to the development of new models and algorithms, pushing the boundaries of AI research. | Collaboration with researchers and experts through open-source platforms fosters innovation and accelerates progress. |
The rise of open-source AI isn’t just a technological trend; it’s a societal shift. By fostering collaboration, transparency, and accessibility, open-source models are democratizing AI and empowering a global community to solve some of our most pressing problems. The journey is ongoing, but the potential for positive impact is undeniable. Let’s continue to explore, innovate, and harness the power of open-source AI for a brighter future.
The more we collaborate, the faster we’ll see groundbreaking solutions emerge, benefitting everyone.