H5N1 Avian Flu A Potential Human Pandemic
H5N1 avian flu could cause a human pandemic – a chilling thought, isn’t it? This highly pathogenic avian influenza virus has been causing outbreaks in birds for years, and while direct human-to-human transmission remains limited, the potential for a global pandemic is a very real concern. The virus’s ability to mutate and its devastating impact on infected individuals make it a serious threat that demands our attention and proactive measures.
We’ll explore the virus’s characteristics, its spread, and what steps are being taken to prevent a catastrophic outbreak.
Understanding H5N1 requires looking at its transmission pathways. While primarily affecting birds, occasional human infections occur through close contact with infected poultry. The severity of these infections varies, but the mortality rate can be alarmingly high. The crucial factor is the potential for the virus to mutate, gaining the ability for efficient human-to-human transmission, a scenario that would rapidly escalate into a pandemic.
H5N1 Avian Flu Virus
The H5N1 avian influenza virus, a subtype of the influenza A virus, poses a significant threat to both poultry populations and, potentially, human health. Understanding its properties and transmission mechanisms is crucial for developing effective prevention and control strategies. While currently not easily transmissible between humans, the potential for mutation and pandemic emergence remains a serious concern.
H5N1 Genetic Makeup and Key Characteristics
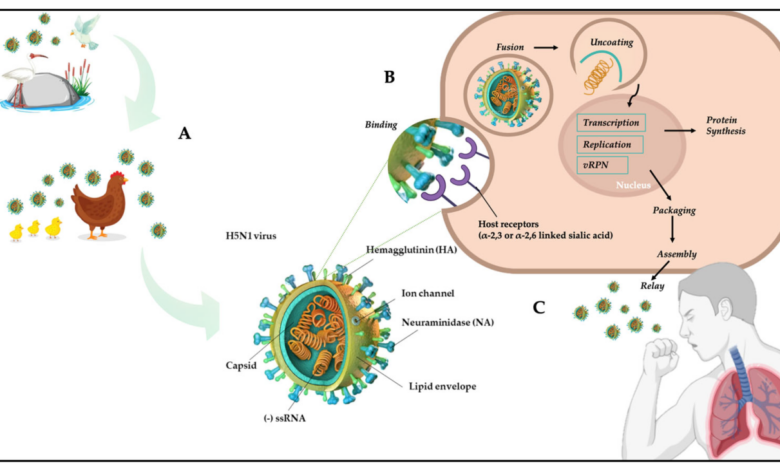
The H5N1 virus, like all influenza A viruses, is an RNA virus with a segmented genome consisting of eight RNA strands. These segments encode various proteins, including hemagglutinin (HA) and neuraminidase (NA), which are crucial for viral entry and release from host cells. The H5 and N1 designations refer to the specific subtypes of HA and NA proteins present on the viral surface.
These proteins are responsible for binding to host cells and facilitating viral replication. The specific genetic makeup of H5N1 strains can vary, leading to differences in virulence and transmissibility. For example, some H5N1 strains exhibit higher pathogenicity in birds, causing more severe disease and higher mortality rates.
H5N1 Transmission Mechanisms
H5N1 primarily circulates among birds, typically through direct contact with infected birds or their droppings. Transmission can also occur through contaminated surfaces or water sources. Human infections are most often associated with direct contact with infected poultry, such as through handling or slaughtering birds. While human-to-human transmission is rare, sporadic cases have been reported, often involving close contact within families.
The exact mechanisms of human-to-human transmission are not fully understood, but it’s believed to require close and prolonged contact, potentially facilitated by factors like crowded living conditions or inadequate hygiene practices. The efficiency of human-to-human transmission remains low compared to other influenza strains.
The H5N1 avian flu’s potential for a human pandemic is genuinely terrifying; imagine the chaos, the overwhelmed healthcare systems. But even in a crisis, accountability remains crucial, which is why understanding how to hold authorities to account is vital – for example, learning how to hold armed police to account in Britain could provide a framework for demanding responsible action during a public health emergency.
Ultimately, preparing for a potential H5N1 pandemic means ensuring robust systems of oversight across all sectors.
Comparison of H5N1 with Other Influenza Strains
Compared to seasonal influenza strains, H5N1 generally exhibits higher virulence in humans, meaning it causes more severe disease. However, its transmissibility between humans is significantly lower. Seasonal influenza strains are easily transmitted through respiratory droplets, leading to widespread outbreaks. In contrast, H5N1 requires closer contact for transmission. The 1918 Spanish flu pandemic, caused by an H1N1 strain, is a stark example of a highly transmissible and virulent influenza virus, causing a global pandemic with high mortality rates.
H5N1, while potentially more lethal in individual cases, has not yet demonstrated the same level of human-to-human transmissibility.
Factors Influencing H5N1 Severity in Humans
The severity of H5N1 infection in humans varies greatly. Several factors influence the outcome of infection, including the specific viral strain, the host’s immune response, and pre-existing health conditions. Individuals with weakened immune systems are at higher risk of developing severe disease. Early intervention with antiviral medications can significantly improve the prognosis. The age of the infected individual is also a factor, with children and the elderly being more vulnerable to severe complications.
Access to quality healthcare plays a critical role in determining the severity of the illness and the chances of survival.
Geographic Distribution and Prevalence of H5N1
The highly pathogenic avian influenza virus H5N1 continues to pose a significant global threat, demanding constant monitoring and proactive measures to prevent potential human pandemics. Understanding its geographic distribution and prevalence is crucial for effective disease control and preparedness strategies. This involves tracking outbreaks in both poultry and humans, identifying high-risk regions, and analyzing the environmental factors that influence its spread.
Global Distribution of H5N1 Outbreaks
Imagine a world map. In recent years, significant outbreaks have been concentrated in several key regions. Southeast Asia, particularly countries like Vietnam, Indonesia, and Cambodia, have experienced persistent outbreaks in poultry, occasionally spilling over into human populations. Similarly, parts of Africa, including Egypt and Nigeria, have seen considerable H5N1 activity. Europe and parts of the Middle East have also reported outbreaks, although often on a smaller scale compared to Asia and Africa.
North America has experienced sporadic outbreaks, primarily affecting poultry populations. A particularly concerning aspect is the increasing spread of H5N1 to previously unaffected regions, highlighting the virus’s adaptability and potential for wider dissemination. The map would visually represent this distribution, with darker shading indicating areas of higher prevalence and clusters of outbreaks.
Regions with Highest Reported Cases
Southeast Asia consistently reports the highest number of H5N1 cases in both poultry and humans. The close proximity of humans to poultry, coupled with the intensive farming practices in some areas, contributes to the higher risk of transmission. Africa also experiences significant outbreaks, particularly in countries with extensive poultry populations and limited biosecurity measures. The precise numbers fluctuate yearly, but these regions consistently remain at the forefront of H5N1 concerns.
The threat of an H5N1 avian flu pandemic looms large, demanding our attention and resources. It’s a scary thought, especially considering the potential economic fallout; we’re already facing potential problems like those highlighted in this article about Biden’s student loan relief plan, bidens student loan relief will lead to severe tax hikes more inflation economists say , which could further strain our ability to respond effectively.
This financial instability could easily hinder our preparedness for a potential avian flu outbreak, making a bad situation even worse.
Detailed data on case numbers, specifying human versus poultry infections, would need to be sourced from reliable epidemiological reports such as those from the World Health Organization (WHO) and the World Organisation for Animal Health (WOAH).
The looming threat of an H5N1 avian flu pandemic keeps me up at night; it’s a global issue demanding immediate attention. It’s unsettling to think about the scale of potential devastation, especially when you consider how easily such crises can expose weaknesses in governance. This reminds me of the political situation in Hungary, where, as reported in this insightful article, peter magyar is reinvigorating hungarys struggling opposition , a strong and effective opposition is crucial during times of crisis – be it political or pandemic-related.
A strong, unified front is essential to effectively combat any large-scale threat like an H5N1 outbreak.
Environmental Factors Contributing to H5N1 Spread
Several environmental factors play a significant role in the spread and persistence of H5N1. Migratory birds are known vectors, carrying the virus across vast distances. Wetland environments, often crucial habitats for migratory birds, can act as reservoirs for the virus. Climate change, leading to altered migratory patterns and increased temperatures, may influence the virus’s geographic range and transmission dynamics.
Furthermore, inadequate biosecurity measures in poultry farms, allowing close contact between wild birds and domestic poultry, facilitate the spread of the virus within poultry populations, increasing the risk of spillover to humans. The density of poultry populations and the proximity of human settlements to poultry farms are also significant risk factors.
H5N1 Outbreaks by Year
| Year | Region | Human Cases | Poultry Cases |
|---|---|---|---|
| 2020 | Southeast Asia, Africa | (Data from WHO/WOAH) | (Data from WHO/WOAH) |
| 2021 | Southeast Asia, Africa, Europe | (Data from WHO/WOAH) | (Data from WHO/WOAH) |
| 2022 | Southeast Asia, Africa, Europe, North America | (Data from WHO/WOAH) | (Data from WHO/WOAH) |
| 2023 | (Data from WHO/WOAH) | (Data from WHO/WOAH) | (Data from WHO/WOAH) |
(Note
This table requires data from reliable sources like the WHO and WOAH to be populated. The bracketed information indicates where this data should be inserted.)*
Public Health Preparedness and Response Strategies

Avian influenza, specifically the H5N1 strain, poses a significant threat to global health security. The potential for a pandemic necessitates a robust and multifaceted public health strategy encompassing preparedness, rapid response, and effective mitigation measures. This strategy must be agile, adaptable, and built upon international collaboration to effectively counter the challenges posed by this highly pathogenic virus.
A Public Health Intervention Strategy to Mitigate H5N1 Pandemic Risk, H5n1 avian flu could cause a human pandemic
An effective intervention strategy requires a layered approach, combining proactive measures with rapid response capabilities. This involves strengthening surveillance systems for early detection, establishing robust healthcare infrastructure to manage potential outbreaks, and developing and deploying effective vaccines and antiviral treatments. Furthermore, public health communication campaigns are crucial to educate the public about preventative measures and reduce fear and misinformation.
Successful implementation necessitates strong governmental leadership, inter-agency coordination, and adequate resource allocation. The strategy must also account for the potential for rapid viral evolution and adaptation, requiring ongoing monitoring and adaptation of control measures. For example, a successful strategy might include pre-positioning of antiviral medications in strategic locations, training healthcare workers in advanced infection control protocols, and establishing clear communication channels to disseminate timely and accurate information to the public.
Preventative Measures for Individuals and Communities
Individual and community-level preventative measures are critical in reducing H5N1 transmission risk. These measures focus primarily on minimizing contact with infected birds. Avoiding contact with poultry, especially sick or dead birds, is paramount. Proper hand hygiene, including frequent handwashing with soap and water, is essential. In areas with known outbreaks, the use of personal protective equipment (PPE), such as masks and gloves, when handling poultry or visiting affected areas, should be considered.
Community-level measures include strengthening biosecurity measures on poultry farms to prevent the spread of the virus among birds and to humans. Public awareness campaigns emphasizing these preventative measures can significantly reduce the risk of infection. For example, a successful community-level campaign might involve distributing educational materials in local languages, utilizing community leaders to spread awareness, and providing access to handwashing facilities in public areas.
Existing Surveillance Systems for Detecting and Monitoring H5N1 Outbreaks
Effective surveillance systems are crucial for early detection and rapid response to H5N1 outbreaks. These systems typically involve active surveillance of poultry populations, including regular testing for the virus. Human surveillance includes monitoring for influenza-like illnesses (ILI) and pneumonia cases, with particular attention to clusters of cases or unusual patterns. Laboratory capacity for rapid and accurate diagnosis is critical.
Data sharing between national and international organizations is essential for tracking the spread of the virus and informing public health interventions. The World Organisation for Animal Health (OIE) and the World Health Organization (WHO) play key roles in coordinating global surveillance efforts. Examples of effective surveillance systems include those implemented in countries with a history of H5N1 outbreaks, where active surveillance in poultry markets and rapid diagnostic testing capacity are well-established.
The Role of International Collaboration in Controlling and Preventing the Spread of H5N1
International collaboration is paramount in controlling and preventing the spread of H5N1. This involves sharing information on outbreaks, coordinating surveillance efforts, and collaborating on the development and deployment of vaccines and antiviral treatments. International organizations like the WHO and the OIE play crucial roles in facilitating this collaboration. Joint research efforts are also essential for better understanding the virus, its evolution, and developing more effective control measures.
International agreements and regulations are crucial to ensure the rapid and effective response to potential pandemics. Examples of successful international collaborations include the sharing of viral samples for research and vaccine development and the coordinated response to outbreaks in multiple countries.
Research and Development Efforts for H5N1: H5n1 Avian Flu Could Cause A Human Pandemic

The ongoing threat of a potential H5N1 avian influenza pandemic necessitates a robust research and development program focused on vaccines, antiviral drugs, and a deeper understanding of the virus itself. Significant progress has been made, but challenges remain in translating laboratory successes into widely available and effective countermeasures.The development of effective H5N1 vaccines and therapeutics is a complex undertaking, hampered by several factors.
These factors demand a multi-pronged approach encompassing basic research, pre-clinical testing, and large-scale clinical trials.
H5N1 Vaccine Development Status
Current research focuses on several vaccine platforms, including inactivated virus vaccines, live attenuated vaccines, and DNA or mRNA vaccines. Inactivated vaccines, while safer, often require multiple doses for optimal efficacy. Live attenuated vaccines offer the potential for stronger immunity with fewer doses, but careful design is crucial to prevent reversion to virulence. DNA and mRNA vaccines offer advantages in terms of rapid production, but their long-term efficacy and safety profiles require further investigation.
Several candidate vaccines have shown promise in pre-clinical trials, but widespread availability remains limited due to production challenges and the need for extensive clinical testing to ensure both safety and effectiveness across diverse populations. For example, a significant hurdle is achieving broad cross-protection against the constantly evolving H5N1 strains.
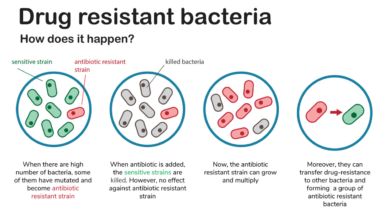
Challenges in Developing Effective H5N1 Vaccines and Antivirals
Developing effective H5N1 countermeasures faces significant challenges. Firstly, the virus’s high mutation rate necessitates the development of vaccines that offer broad protection against various strains. Secondly, the logistical challenges of producing and distributing vaccines globally, especially to resource-limited settings, are immense. Thirdly, ensuring equitable access to vaccines and antivirals is a critical ethical and public health consideration.
Finally, predicting which strains will be most prevalent in the future remains a challenge, impacting vaccine strain selection and efficacy. For instance, the rapid evolution of H5N1 subtypes necessitates continuous monitoring and adaptation of vaccine strategies.
Understanding H5N1 Virus Evolution and Adaptation
Ongoing research is crucial to understanding the evolutionary dynamics of the H5N1 virus. This includes genomic surveillance to track mutations and identify potential pandemic strains. Studies are investigating the factors that contribute to viral adaptation, such as host immune pressure and environmental factors. This knowledge is essential for developing more effective vaccines and antiviral strategies that can anticipate and counter future evolutionary changes.
For example, detailed analysis of viral sequences from different geographic regions helps researchers understand the emergence of novel strains and predict potential pandemic threats.
Latest Scientific Findings on H5N1 Pathogenicity and Transmission
Recent research has provided insights into the pathogenicity and transmission of H5N1. Studies have identified specific viral genes and proteins responsible for its virulence and ability to infect humans. Research is also focused on understanding the factors influencing human-to-human transmission, which remains relatively rare but poses a significant pandemic risk. Improved understanding of these mechanisms is essential for developing targeted interventions to reduce the severity of infection and prevent transmission.
For example, studies have identified specific mutations associated with increased virulence and transmissibility, informing the development of more effective diagnostic tools and antiviral strategies.
The threat of an H5N1 pandemic is a stark reminder of our vulnerability to emerging infectious diseases. While current human-to-human transmission remains limited, the potential for a devastating outbreak necessitates ongoing vigilance and proactive measures. Investing in research, developing effective vaccines and antiviral treatments, and strengthening global surveillance systems are critical steps in mitigating this risk. Staying informed and practicing preventative measures are also crucial roles we all play in protecting ourselves and our communities.
The future may hold uncertainty, but proactive preparedness offers the best chance to prevent a catastrophic scenario.