Mpox in Africa Pandemic Potential?
Mpox is raging across africa could it become a pandemic – Mpox is raging across Africa: could it become a pandemic? That’s the chilling question on many minds. This isn’t just another news headline; it’s a story unfolding in real-time, impacting communities across the continent. We’ll delve into the current situation, exploring the factors driving the spread, the challenges in containing it, and the very real possibility of a global health crisis.
Get ready for a deep dive into a situation that demands our attention.
The sheer scale of the outbreak is alarming. From tracking the virus’s geographical spread across various nations to understanding the demographics most affected, the challenges are immense. We’ll examine the role of healthcare infrastructure, social factors, and the effectiveness of public health responses. Are we prepared for what might come next? The answer, unfortunately, is complex and requires careful consideration of various factors.
Current Mpox Situation in Africa
The recent resurgence of mpox, formerly known as monkeypox, in Africa presents a complex public health challenge. While the global attention initially focused on outbreaks in non-endemic regions, the ongoing situation in Africa demands careful consideration, particularly given the limitations in surveillance and resource allocation. Understanding the current epidemiological landscape is crucial for effective response and prevention strategies. This requires a nuanced understanding of the geographical distribution, affected demographics, and challenges in data collection across diverse African settings.
Geographical Distribution of Mpox Cases in Africa
Accurately tracking mpox cases across Africa is challenging due to variations in surveillance capacity and reporting systems. The following table provides a snapshot of the situation, acknowledging that data may be incomplete or delayed. It is vital to remember that this data represents a minimum number of cases, and the actual numbers are likely higher due to underreporting.
| Country | Number of Cases (Approximate) | Date of Last Reported Case (Approximate) | Public Health Response |
|---|---|---|---|
| Democratic Republic of Congo | Several thousand (exact numbers vary widely depending on the source and time of reporting) | Ongoing | Limited resources; ongoing vaccination campaigns in high-risk areas; community engagement and awareness programs. |
| Nigeria | Hundreds (exact numbers vary widely depending on the source and time of reporting) | Ongoing | Surveillance efforts and contact tracing; limited vaccine availability; public health messaging campaigns. |
| Cameroon | Dozens (exact numbers vary widely depending on the source and time of reporting) | Ongoing | Limited data; surveillance and response efforts hampered by limited resources. |
| Other Central and West African Countries | Sporadic cases reported | Ongoing | Variable; depends on country-specific capacities and resources. |
Demographics of Those Affected by Mpox in Africa
The demographic profile of mpox cases varies across different regions of Africa, highlighting the need for tailored interventions. Factors such as access to healthcare, cultural practices, and socioeconomic conditions significantly influence the spread and impact of the disease.
The following points illustrate some of the observed demographic trends, keeping in mind that data availability and quality varies across countries:
- In many regions, a significant proportion of cases are among young adults, although the age range varies.
- While mpox traditionally affects males more often, this is not consistently observed across all African countries, and the gender distribution needs further investigation in many areas.
- Rural populations often face greater challenges in accessing healthcare and are thus more vulnerable to severe outcomes.
- The impact of socioeconomic factors on mpox incidence and mortality requires further investigation in different African contexts.
Challenges in Tracking and Reporting Mpox Cases in Africa
Several factors hinder accurate and timely tracking and reporting of mpox cases in various African countries. These challenges are interconnected and often exacerbate each other, leading to underreporting and a less effective public health response.
These challenges include:
- Limited diagnostic capacity: Many countries lack sufficient laboratory capacity for timely and accurate diagnosis of mpox.
- Weak surveillance systems: Existing surveillance systems may not be robust enough to detect and track all cases, particularly in remote areas.
- Inadequate healthcare infrastructure: Limited access to healthcare, especially in rural areas, can hinder early detection and treatment.
- Resource constraints: Financial and human resource limitations hamper effective surveillance, response, and prevention efforts.
- Social and cultural factors: Stigma and fear surrounding the disease can discourage individuals from seeking medical care or reporting cases.
Factors Contributing to Mpox Spread in Africa
The current mpox outbreak in Africa, while distinct from the 2022 global outbreak, highlights the complex interplay of social, economic, and infrastructural factors that influence the spread of the virus. Understanding these factors is crucial for developing effective prevention and control strategies tailored to the specific contexts of affected African communities. This analysis will explore some of the key contributors to the ongoing spread.
Several interconnected factors contribute to the spread of mpox within African communities. These factors often intersect and exacerbate each other, creating a challenging environment for disease control.
Mpox cases are surging in Africa, raising serious concerns about a potential global pandemic. It’s a stark reminder of how quickly infectious diseases can spread, and honestly, it makes me think about how easily things can be manipulated for political gain, like the situation Katie Pavlich highlights, where she claims Tlaib and Omar purposely timed their Israel trip to cause controversy.
The parallels between the potential spread of mpox and the deliberate creation of political controversy are unsettling; both situations demand our attention and responsible action.
Socioeconomic Factors Influencing Mpox Transmission
Limited access to resources and information plays a significant role. Poverty, food insecurity, and lack of education can hinder individuals’ ability to understand and practice preventative measures. For example, in rural communities with limited access to healthcare, information about mpox symptoms and transmission may not reach the population effectively, delaying diagnosis and treatment. Furthermore, cultural practices, such as close physical contact during traditional ceremonies or communal living arrangements, can increase the risk of transmission, especially in areas with high population density and limited sanitation.
These socio-economic disparities often lead to unequal access to healthcare, testing, and treatment, further contributing to the spread of the virus. For instance, individuals in marginalized communities may face barriers in accessing testing and treatment due to cost, geographical location, or stigma associated with the disease.
The Role of Healthcare Infrastructure and Access
Inadequate healthcare infrastructure and limited access to quality healthcare services are significant obstacles in controlling mpox outbreaks in Africa. Many regions lack sufficient healthcare facilities, trained medical personnel, and diagnostic tools necessary for early detection and effective management of cases. This delay in diagnosis and treatment can lead to increased transmission within communities. The shortage of personal protective equipment (PPE) for healthcare workers further compounds the problem, putting both healthcare workers and patients at risk.
Moreover, weak surveillance systems hamper the ability to track and monitor the spread of the virus effectively, making it challenging to implement targeted interventions. A lack of robust public health infrastructure, including effective contact tracing and isolation facilities, makes it difficult to contain outbreaks effectively.
Comparison with Previous Mpox Outbreaks
The current outbreak in Africa differs from previous outbreaks in several key aspects. While previous outbreaks were often localized and contained within specific regions, the current situation shows a wider geographical spread across multiple countries. Previous outbreaks also often involved smaller numbers of cases, while the current situation presents a larger scale challenge. The 2022 global outbreak, while primarily impacting non-African countries, highlighted the potential for rapid international spread, a factor that necessitates a heightened level of vigilance in Africa.
The differences in the scale and spread underscore the need for tailored strategies that address the unique challenges presented by the current outbreak in Africa, recognizing the existing vulnerabilities in healthcare systems and socio-economic conditions.
Public Health Response and Preparedness
The current mpox outbreak in Africa highlights the critical need for robust and adaptable public health interventions. While significant challenges exist, including limited resources and healthcare infrastructure, several initiatives are underway, with varying degrees of success. A comprehensive evaluation of these efforts is crucial to inform future strategies and optimize resource allocation for effective disease control.The effectiveness of current public health interventions in affected African countries is a complex issue.
Many nations lack the resources for widespread testing, contact tracing, and vaccination campaigns. Furthermore, existing health systems often struggle with basic healthcare provision, making the implementation of mpox-specific interventions even more challenging. While some countries have successfully implemented targeted vaccination campaigns in high-risk groups, the overall reach remains limited. Data collection and reporting systems also vary widely across the continent, hindering a comprehensive understanding of the outbreak’s true scale and impact.
Successful interventions have often relied on strong community engagement, leveraging existing networks and trusted community leaders to disseminate information and encourage safe practices. However, this approach requires significant investment in community health workers and sustained engagement.
Effectiveness of Current Public Health Interventions, Mpox is raging across africa could it become a pandemic
Several factors influence the effectiveness of current public health responses. These include the availability of diagnostic tools, the capacity for contact tracing, the accessibility of treatment and vaccines, and the overall strength of the healthcare system. In many affected African countries, limited resources and infrastructure hinder the implementation of effective control measures. For example, the lack of sufficient testing capacity can lead to underreporting of cases, making it difficult to accurately assess the extent of the outbreak and allocate resources appropriately.
Similarly, limited access to vaccines and antiviral treatments exacerbates the challenges in controlling the spread of the virus. Effective interventions often rely on collaborative efforts between national governments, international organizations, and local communities.
Designing a Public Awareness Campaign
A comprehensive public awareness campaign is vital to effectively control the spread of mpox. This campaign should utilize multiple channels, including radio, television, social media, and community-based outreach programs. Key messages should focus on simple, clear, and actionable steps that individuals can take to protect themselves and others.The target audiences for this campaign should include diverse groups within the affected communities, with tailored messaging to address specific concerns and cultural contexts.
Seriously, the mpox outbreak in Africa is terrifying; it feels like we’re constantly battling one global health crisis after another. And while I’m trying to keep up with that, I also saw this completely unrelated news story about trump files motion seeking to prevent doj access to mar a lago records until special master appointed , which, honestly, just adds to the general sense of chaos.
It makes you wonder if we have the resources to handle everything properly, especially given the potential for a wider mpox pandemic.
This includes men who have sex with men (MSM), healthcare workers, community leaders, and the general population. For example, messages targeted at MSM might emphasize safe sex practices and the importance of seeking medical attention if symptoms develop. Messages directed towards healthcare workers would focus on infection prevention and control measures in healthcare settings. Community leaders can play a crucial role in disseminating information and promoting adherence to public health guidelines.
Key Messages for the Public Awareness Campaign
The campaign’s key messages should be consistent, easy to understand, and culturally sensitive. Examples include:
- Mpox is a viral disease that can spread through close contact.
- Practice good hygiene, including frequent handwashing.
- Avoid close contact with individuals showing symptoms.
- Seek medical attention if you experience symptoms.
- Vaccination is available and can help protect you.
Best Practices from Other Regions
Several best practices from other regions, such as successful mpox control efforts in Europe and North America, can be adapted to the African context. These include the use of effective communication strategies, community engagement, and the establishment of strong surveillance systems. However, adapting these practices requires careful consideration of the unique challenges faced by African countries, including limited resources, healthcare infrastructure, and cultural factors.
For instance, successful contact tracing strategies in high-income countries may need to be modified to suit the realities of resource-constrained settings in Africa. The emphasis should be on community-based approaches, utilizing existing community structures and networks for effective dissemination of information and implementation of control measures. Successful implementation necessitates culturally sensitive communication, incorporating local languages and customs to ensure effective engagement and compliance.
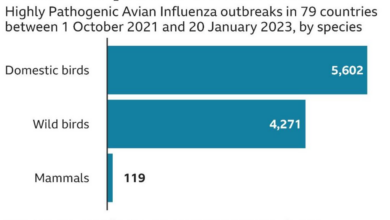
Potential for a Global Pandemic
The current mpox outbreak in Africa raises serious concerns about its potential to escalate into a global pandemic. While the immediate threat is concentrated in the African continent, several factors could facilitate its widespread international transmission, mirroring or exceeding the impact of previous outbreaks. Understanding these factors is crucial for implementing effective prevention and control strategies.The risk of a global mpox pandemic hinges on several interconnected elements.
Increased international travel and trade could rapidly disseminate the virus to regions with limited public health infrastructure or high population densities, potentially leading to uncontrolled outbreaks. Furthermore, the emergence of new variants with increased transmissibility or virulence poses a significant threat. Finally, complacency and inadequate global preparedness could significantly hamper effective response efforts.
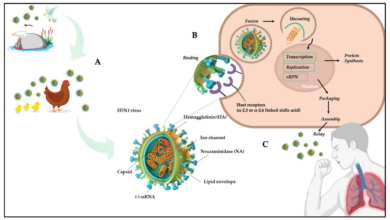
Transmissibility and Virulence of the Current Strain
The current mpox strain circulating in Africa exhibits characteristics that warrant close monitoring. While the exact transmissibility and virulence remain subjects of ongoing research, comparative analysis with previous strains is essential. Early data suggests that the current strain might display slightly higher transmissibility than some previous strains, though definitive conclusions require further investigation. This increased transmissibility, coupled with potential variations in virulence, could significantly influence the pandemic potential.
For instance, if a variant emerges with higher virulence and prolonged contagiousness, the potential for rapid spread would dramatically increase, as seen with other infectious diseases throughout history. The 2003 SARS outbreak, for example, highlighted the speed with which a novel and highly transmissible virus can spread globally, despite initial containment efforts.
Potential Escalation Scenarios
Several scenarios could lead to a global mpox pandemic originating from Africa.
Scenario 1: A highly transmissible variant emerges in a densely populated African city with significant international travel connections. Rapid spread within the city is followed by export to multiple global hubs, overwhelming local and international health systems.
Scenario 2: Multiple, simultaneous outbreaks occur across different African countries, exceeding the capacity of local health systems to contain the virus. International travel and trade then contribute to widespread global dissemination, before effective containment measures can be implemented.
Scenario 3: The current strain, without significant mutation, gains a foothold in a region with low vaccination rates and weak public health infrastructure. This leads to sustained transmission, creating a reservoir for further spread through international travel and trade. This could be exacerbated by a lack of widespread awareness and appropriate preventative measures within the affected population.
Scenario 4: A novel mpox strain emerges that exhibits significantly increased transmissibility and virulence, potentially even bypassing existing immunity. Rapid global spread ensues, overwhelming even well-resourced healthcare systems.
These scenarios highlight the importance of proactive surveillance, rapid response mechanisms, and international collaboration to mitigate the risk of a global mpox pandemic. The lessons learned from previous outbreaks, such as Ebola and COVID-19, underscore the need for robust public health infrastructure and effective communication strategies to prevent and control the spread of infectious diseases. These scenarios are not predictions, but rather illustrations of potential pathways based on the current understanding of mpox transmission and the dynamics of previous pandemics.
The mpox outbreak in Africa is deeply concerning; its potential to become a global pandemic is a very real threat. It’s a reminder that global health crises demand international cooperation, and the geopolitical landscape plays a huge role. For example, consider how a potential Trump win impacts this, as outlined in this insightful article: what trumps win means for china , because shifts in global power dynamics inevitably affect resource allocation and international collaborations crucial for tackling pandemics like mpox.
Ultimately, the future of mpox control depends on many factors, including global leadership and collaboration.
Effective preparedness and swift action are key to preventing these scenarios from becoming reality.
Research and Development Needs
The current mpox outbreak in Africa highlights critical gaps in our understanding of the virus and our capacity to effectively respond. Addressing these gaps requires a significant investment in research and development, focusing on diagnostics, therapeutics, and vaccine development tailored to the African context. This investment is crucial not only for controlling the current outbreak but also for preventing future ones.The urgent need for improved diagnostics, treatments, and vaccines is undeniable.
Current diagnostic methods can be expensive, require specialized equipment and trained personnel, and may not be readily available in many parts of Africa. Similarly, treatment options are limited, and existing vaccines may not offer optimal protection against all circulating strains. Therefore, research must focus on developing affordable, accessible, and effective tools for mpox prevention and control.
Diagnostic Tool Development
Rapid, point-of-care diagnostic tests are essential for early detection and isolation of infected individuals, thereby limiting transmission. Current PCR-based tests, while accurate, often require sophisticated laboratory infrastructure and trained personnel, limiting their accessibility in many African settings. Research should focus on developing simpler, cheaper, and more robust diagnostic tools, such as lateral flow assays (LFAs) similar to those used for rapid malaria or HIV testing.
These tests should ideally be adaptable to different resource settings and capable of detecting various mpox strains. A successful LFA would need to demonstrate high sensitivity and specificity in field trials, ensuring accurate results even in challenging conditions. The development of such a test would revolutionize mpox surveillance and control efforts in Africa.
Therapeutic Development
Existing antiviral treatments, such as tecovirimat, have shown some efficacy against mpox, but their accessibility and affordability remain major challenges in resource-limited settings. Research should focus on developing more affordable and accessible antiviral drugs, possibly through repurposing existing medications or exploring novel therapeutic targets. Furthermore, studies investigating the efficacy of traditional medicine practices used in some African communities to manage mpox symptoms should be conducted rigorously to determine their potential value and safety.
These studies should follow internationally recognized ethical guidelines and include robust data collection methods. For example, a randomized controlled trial comparing the efficacy of a novel antiviral drug to a placebo, while adhering to strict ethical standards and data collection, could provide invaluable information.
Vaccine Development and Optimization
While existing smallpox vaccines offer some cross-protection against mpox, their efficacy may vary against different mpox strains, and they carry potential side effects. Research is needed to develop mpox-specific vaccines that are safe, effective, and easily deployable in resource-limited settings. This includes exploring different vaccine platforms, such as mRNA or viral vector vaccines, and optimizing vaccine delivery strategies to ensure high coverage in vulnerable populations.
Research should also investigate the duration of immunity provided by different vaccine candidates and the potential need for booster doses. A clinical trial comparing the efficacy and safety of a novel mpox vaccine to a smallpox vaccine in a diverse African population would be a significant contribution to the field.
Challenges in Conducting Research in Resource-Limited Settings
Conducting research and clinical trials in resource-limited settings presents numerous challenges. These include limited infrastructure, funding constraints, logistical difficulties, and ethical considerations. The lack of well-equipped laboratories, trained personnel, and reliable transportation can significantly hinder research activities. Securing adequate funding for research projects can also be challenging, as many African countries face limited resources for health research.
Furthermore, ethical considerations, such as informed consent and data privacy, need careful attention, especially in communities with limited literacy levels. Addressing these challenges requires collaborative efforts between international research institutions, African governments, and local communities.
Hypothetical Research Proposal: Investigating Mpox Transmission Dynamics in Rural Communities
This study aims to investigate the transmission dynamics of mpox in rural communities in [Specific Region of Africa], focusing on the role of animal reservoirs and human-to-human transmission routes. The study will employ a mixed-methods approach, combining epidemiological surveys, serological testing, and environmental sampling. The epidemiological surveys will collect data on mpox cases, contact tracing, and potential risk factors.
Serological testing will determine the prevalence of mpox antibodies in human and animal populations. Environmental sampling will identify potential viral reservoirs in the environment. The data collected will be analyzed to construct a transmission model to predict the spread of mpox under different scenarios and inform public health interventions. This research will provide crucial data to inform targeted interventions and improve mpox control strategies in rural African communities.
International Collaboration and Support: Mpox Is Raging Across Africa Could It Become A Pandemic
The mpox outbreak in Africa highlights the critical need for robust international collaboration to effectively control the virus and prevent its further spread. A coordinated global response, built on equitable partnerships and resource sharing, is essential to mitigate the impact of this public health emergency. Failure to act decisively and collaboratively will not only prolong the suffering in affected African nations but also increase the risk of a global pandemic.The role of international organizations in supporting African countries’ efforts is multifaceted and crucial.
These organizations, including the World Health Organization (WHO), the African Union (AU), and various bilateral partners, provide vital technical assistance, financial resources, and logistical support. This includes epidemiological surveillance, laboratory capacity building, vaccine procurement and distribution, and public health communication strategies. However, the effectiveness of this support hinges on equitable access to resources and a commitment to fostering strong, collaborative relationships with national governments.
Equitable Access to Mpox Resources
Ensuring equitable access to vaccines, treatments, and diagnostics is paramount for controlling the mpox outbreak in Africa. Historically, inequities in global health resource distribution have disproportionately affected low- and middle-income countries. The mpox outbreak underscores this persistent challenge. A fair and just distribution mechanism is needed, prioritizing vulnerable populations and ensuring that African nations have sufficient supplies to meet their needs.
This requires not only financial resources but also robust logistical networks to overcome challenges such as limited infrastructure and transportation difficulties in some regions. For example, the successful deployment of the COVID-19 vaccine demonstrated the power of international collaboration, but also revealed the shortcomings in equitable access for many nations, a lesson that must be applied to the current mpox situation.
Framework for Effective International Collaboration
An effective framework for international collaboration to address the mpox outbreak in Africa should be based on several key principles. First, it must be built on a foundation of mutual respect and shared responsibility. This means actively involving African nations in all stages of the response, from planning and implementation to evaluation and monitoring. Second, transparency and accountability are crucial.
Information sharing, including epidemiological data and research findings, must be open and accessible to all partners. Third, the framework must prioritize sustainable capacity building. This involves investing in local expertise and infrastructure to strengthen African nations’ long-term ability to respond to public health emergencies. Finally, a dedicated funding mechanism is essential, ensuring that resources are allocated efficiently and effectively to address immediate needs and build long-term resilience.
This might involve a coordinated international fund specifically designed to address mpox in Africa, leveraging existing global health initiatives and building on lessons learned from previous outbreaks. A clear allocation process with transparent metrics for evaluating impact is also vital.
The mpox outbreak in Africa is a stark reminder of the interconnectedness of our world and the fragility of global health security. While the potential for a pandemic is a serious concern, understanding the current situation, supporting affected communities, and investing in research and prevention are crucial steps. This isn’t just about containing a virus; it’s about addressing systemic inequalities and building stronger, more resilient health systems, both in Africa and globally.
The fight against mpox is a fight for global health equity, and it’s a fight we must win.