New Fronts Are Opening in the War Against Malaria
New fronts are opening in the war against malaria, and the fight is far from over! This isn’t just about mosquito nets anymore; we’re talking groundbreaking gene drives, innovative new drugs, and a much-needed focus on the social and economic factors fueling this deadly disease. It’s a complex battle, but the advancements being made are genuinely inspiring.
From tackling the limitations of traditional insecticide-treated nets to exploring the ethical implications of gene editing, the scientific community is pushing boundaries. Simultaneously, we’re finally acknowledging the crucial role of poverty, lack of healthcare access, and climate change in malaria’s persistence. It’s a holistic approach, recognizing that defeating malaria requires a multi-pronged attack, addressing both the scientific and societal challenges head-on.
Addressing the Socioeconomic Factors Contributing to Malaria Prevalence: New Fronts Are Opening In The War Against Malaria

Malaria’s persistence is deeply intertwined with socioeconomic factors that create a breeding ground for the disease. Understanding these complex relationships is crucial for developing effective and sustainable interventions. Poverty, limited access to healthcare, and inadequate sanitation all play significant roles in perpetuating the malaria cycle, disproportionately affecting vulnerable populations.
Exciting new fronts are opening in the war against malaria, with innovative gene drives and advanced diagnostics showing real promise. It makes you wonder about resource allocation – are we seeing a similar surge of innovation in other areas? I was reading this fascinating article on whether America is approaching peak tip, is america approaching peak tip , which got me thinking about how we prioritize global health challenges like malaria against other societal pressures.
Ultimately, the fight against malaria needs continued investment and focus to truly win.
The correlation between socioeconomic factors and malaria prevalence is undeniable. Poverty often forces individuals to live in environments conducive to mosquito breeding, such as areas with stagnant water and poor sanitation. Lack of access to healthcare prevents early diagnosis and treatment, allowing infections to progress and potentially become life-threatening. Inadequate sanitation further exacerbates the problem by providing breeding grounds for mosquitoes and increasing the risk of transmission.
Exciting new fronts are opening in the war against malaria, with innovative gene drives and advanced diagnostics showing real promise. It makes me think of the tech world – while breakthroughs happen, sometimes even giants like Masayoshi Son, as discussed in this article masayoshi son is back in silicon valley and late to the ai race , can find themselves playing catch-up.
But the fight against malaria, thankfully, continues to advance relentlessly on multiple fronts.
Socioeconomic Factors and Malaria Rates, New fronts are opening in the war against malaria
The following table illustrates the strong correlation between socioeconomic factors and malaria rates. While precise correlations vary depending on location and specific contexts, the general trend is clear.
| Factor | Correlation with Malaria Rates | Solutions |
|---|---|---|
| Poverty | High correlation; impoverished communities often lack resources for mosquito control and treatment. | Targeted poverty reduction programs, including cash transfers and improved access to employment opportunities. Investment in infrastructure to improve housing and sanitation. |
| Lack of Access to Healthcare | Strong correlation; delayed or absent treatment leads to increased morbidity and mortality. | Increased investment in healthcare infrastructure, including community health centers and mobile clinics. Training and deployment of healthcare workers, particularly in remote areas. Improved access to affordable antimalarial drugs. |
| Inadequate Sanitation | High correlation; stagnant water and unsanitary conditions provide ideal breeding grounds for mosquitoes. | Improved sanitation infrastructure, including waste management systems and access to clean water. Community-based sanitation programs promoting hygiene practices. |
Climate Change and Malaria Transmission
Climate change is significantly altering malaria transmission patterns and geographic distribution. Rising temperatures, changes in rainfall patterns, and increased humidity expand the suitable habitat for malaria-carrying mosquitoes, potentially leading to outbreaks in previously unaffected regions. Moreover, changes in temperature can influence mosquito development rates and lifespan, affecting transmission intensity.
A visual representation of projected changes in malaria risk zones would show a map with shaded areas indicating varying levels of risk. Areas currently at low risk might become high-risk zones, depicted by darker shading, while existing high-risk zones could intensify. The map would illustrate the expansion of malaria risk into new geographic regions and the increased intensity in already affected areas, highlighting the need for proactive adaptation strategies.
The fight against malaria is gaining momentum with exciting new breakthroughs in vaccine development and innovative vector control strategies. Successfully implementing these requires strong leadership, and that’s where understanding what makes a good manager comes in; check out this insightful article on what makes a good manager for some key insights. Ultimately, effective management is crucial for coordinating these diverse efforts and ensuring these new fronts in the malaria war truly deliver impactful results.
Community Engagement Strategies for Malaria Prevention and Control
Engaging communities is paramount to successful malaria prevention and control efforts. Community participation ensures the sustainability of interventions and fosters a sense of ownership among the population most affected.
- Community-based health education programs: These programs use various methods, including workshops, community meetings, and interactive sessions, to educate people about malaria prevention, early detection, and treatment. They emphasize practical measures such as using insecticide-treated nets, indoor residual spraying, and seeking prompt medical attention.
- Active community participation in mosquito control: This involves empowering communities to actively participate in mosquito control activities, such as cleaning up breeding sites, removing stagnant water, and maintaining proper sanitation. This fosters a sense of responsibility and collective action.
- Strengthening partnerships with community leaders and organizations: Collaboration with local leaders, religious institutions, and community-based organizations ensures effective dissemination of information and facilitates the implementation of interventions tailored to specific community needs and cultural contexts. This collaborative approach enhances program acceptance and impact.
Improving Malaria Surveillance and Diagnostics

Effective malaria control hinges on robust surveillance and accurate diagnosis. Without these crucial components, efforts to prevent and treat the disease are significantly hampered, leading to continued suffering and potential outbreaks. Understanding the complexities of malaria transmission and developing targeted interventions require a comprehensive understanding of where and when the disease is occurring, and who is affected. This necessitates a multifaceted approach to surveillance and diagnostics.
Malaria Surveillance Systems
Robust surveillance systems are vital for detecting and responding to malaria outbreaks. Early detection allows for timely implementation of control measures, minimizing the spread of the disease and reducing morbidity and mortality. A well-designed surveillance system provides critical data on malaria epidemiology, informing public health decisions and resource allocation. The following flowchart illustrates a typical malaria surveillance system:
Flowchart: Malaria Surveillance System
Step 1: Data Collection
– This involves collecting data from various sources, including routine health facility reporting, community health workers, and mobile health technologies. Data points typically include the number of suspected and confirmed malaria cases, age and sex of patients, geographic location, and date of onset of symptoms.
Step 2: Data Analysis
-Collected data is analyzed to identify trends, patterns, and outbreaks. This may involve calculating malaria incidence rates, mapping disease distribution, and identifying high-risk populations.
Step 3: Alert and Response
– When an outbreak or unusual increase in malaria cases is detected, an alert is triggered. This triggers a rapid response, which may include deploying additional health workers, distributing insecticide-treated bed nets, and implementing targeted vector control measures.
Step 4: Evaluation
-The effectiveness of the response is evaluated to improve future interventions. This involves monitoring the impact of implemented measures on malaria incidence and transmission.
Step 5: Feedback and Improvement
-Feedback from the evaluation process is used to improve the surveillance system’s efficiency and effectiveness. This may involve refining data collection methods, enhancing analytical capabilities, and strengthening response mechanisms.
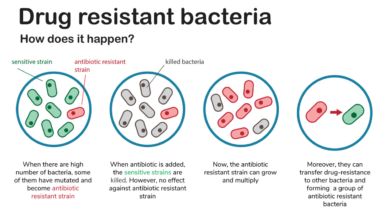
Malaria Diagnostic Methods
Accurate and timely diagnosis is crucial for effective malaria management. Various diagnostic methods exist, each with its advantages and disadvantages:
| Method | Advantages | Disadvantages |
|---|---|---|
| Microscopy | Relatively inexpensive, widely available, can identify the species of Plasmodium | Requires skilled microscopists, time-consuming, less sensitive than other methods, can be subjective |
| Rapid Diagnostic Tests (RDTs) | Rapid results, easy to use, no specialized equipment needed, suitable for point-of-care testing | Lower sensitivity and specificity compared to PCR, potential for false positive or negative results, affected by temperature and humidity |
| Polymerase Chain Reaction (PCR) | Highly sensitive and specific, can detect low parasite densities, can identify the species of Plasmodium | Expensive, requires specialized equipment and trained personnel, not suitable for point-of-care testing |
Challenges in Accessing Rapid Diagnostic Tests
Rapid diagnostic tests (RDTs) are crucial for timely diagnosis and treatment of malaria, especially in remote areas. However, several challenges hinder their accessibility:
The effective deployment of RDTs in remote and underserved areas faces significant hurdles. Overcoming these obstacles requires a multi-pronged approach involving logistical improvements, training programs, and community engagement.
- Challenge 1: Inadequate supply chain infrastructure: Poor roads, lack of refrigeration, and unreliable transportation networks can lead to shortages and spoilage of RDTs.
- Solution 1: Invest in robust cold chain logistics, including the use of solar-powered refrigerators and improved transportation networks. Establish reliable supply chains with regular stock replenishment.
- Challenge 2: Lack of trained healthcare workers: The proper use and interpretation of RDTs require adequate training. A shortage of trained personnel can lead to misdiagnosis and inappropriate treatment.
- Solution 2: Implement comprehensive training programs for healthcare workers in remote areas. Utilize mobile technology and distance learning to enhance accessibility to training materials.
- Challenge 3: High cost of RDTs: The cost of RDTs can be prohibitive in resource-limited settings, especially for individuals and communities with limited financial resources.
- Solution 3: Explore cost-effective procurement strategies, including bulk purchasing and government subsidies. Promote the use of generic RDTs where appropriate and quality is assured.
Strengthening Global Collaboration and Funding for Malaria Eradication

The fight against malaria requires a concerted global effort, transcending national borders and individual initiatives. Success hinges on robust collaboration between nations, international organizations, and research institutions, coupled with substantial and sustained funding. This section explores the crucial roles played by global partnerships and the financial landscape in shaping the future of malaria control.The Role of International Organizations in Coordinating Global Malaria Control EffortsInternational organizations play a vital coordinating role in the global fight against malaria.
The World Health Organization (WHO), for example, provides technical guidance, sets global strategies, and monitors progress towards malaria eradication goals. The Global Fund to Fight AIDS, Tuberculosis and Malaria is a crucial funding mechanism, channeling resources to countries most affected by the disease. The Bill & Melinda Gates Foundation also plays a significant role, investing heavily in research and development, as well as supporting implementation programs on the ground.
Successful collaborative initiatives include the Roll Back Malaria (RBM) partnership, a broad coalition of public and private organizations working together to reduce the global malaria burden. The RBM partnership has facilitated the sharing of best practices, coordinated advocacy efforts, and mobilized resources for malaria control programs worldwide. Another example is the development and deployment of insecticide-treated mosquito nets, a collaborative effort involving numerous organizations and governments, leading to a significant reduction in malaria cases in many regions.The Funding Landscape for Malaria Research and ControlThe funding landscape for malaria research and control is complex, involving a diverse range of donors and funding priorities.
Major donors include governments (such as the United States, the United Kingdom, and several European nations), philanthropic organizations (like the Bill & Melinda Gates Foundation and the Wellcome Trust), and multilateral organizations (like the Global Fund). Funding priorities often reflect the current state of the disease burden, focusing on areas with the highest malaria transmission rates and most vulnerable populations.
A significant portion of funding is directed towards vector control (e.g., insecticide-treated nets, indoor residual spraying), followed by case management (including rapid diagnostic tests and artemisinin-based combination therapies). Research and development also receive considerable funding, although it often falls short of the level required to develop new and effective tools.A hypothetical bar graph illustrating the distribution of funding among different malaria control strategies would show the largest bar representing vector control, followed by a slightly smaller bar for case management.
A smaller bar would represent research and development, and even smaller bars would depict surveillance, community engagement, and other strategies. The precise proportions would depend on the specific year and data source.The Impact of Inadequate Funding on Malaria Control Programs and Strategies to Secure Increased and Sustainable FundingInadequate funding significantly hampers malaria control programs. It can lead to shortages of essential medicines, diagnostic tools, and trained personnel.
It can also limit the scale-up of effective interventions and hinder research efforts to develop new tools and strategies. This ultimately results in continued high rates of malaria morbidity and mortality, particularly in resource-limited settings. Securing increased and sustainable funding is crucial for achieving malaria eradication goals.To achieve this, several strategies can be employed:
- Strategy 1: Strengthen advocacy efforts to raise awareness among governments and the public about the devastating impact of malaria and the need for increased investment in control programs. This involves highlighting the economic benefits of malaria eradication, such as increased productivity and reduced healthcare costs.
- Strategy 2: Diversify funding sources beyond traditional donors by exploring innovative financing mechanisms, such as impact investing, public-private partnerships, and philanthropic initiatives. This would reduce reliance on a few key donors and enhance the long-term sustainability of funding.
- Strategy 3: Improve the efficiency and transparency of malaria funding mechanisms to ensure that resources are used effectively and accountability is maintained. This includes strengthening monitoring and evaluation systems to track progress and demonstrate the impact of investments.
The fight against malaria is far from won, but the opening of these new fronts offers a renewed sense of hope. The convergence of technological advancements, a deeper understanding of socioeconomic factors, improved surveillance, and strengthened global collaboration is creating a powerful synergy. While challenges remain, the innovative spirit and collaborative efforts currently underway promise a future where malaria is no longer a global health crisis.
It’s a marathon, not a sprint, but we’re making progress, and that’s something to celebrate.